Summary: Vitamin D causes dendritic cells to produce more CD31, hindering the activation of T cells. The study sheds light on how vitamin D deficiency regulates the immune system and can lead to autoimmune diseases, like multiple sclerosis.
Source: University of Edinburgh
Scientists have uncovered fresh insights into how vitamin D affects the immune system and might influence susceptibility to diseases such as multiple sclerosis.
Vitamin D is produced by the body in response to sunlight and is often lauded for its health benefits. Researchers found it also affects key cells of the immune system.
This discovery might explain how vitamin D regulates immune reactions that have been implicated in autoimmune diseases such as MS.
The University of Edinburgh team focused on how vitamin D affects a mechanism in the body’s immune system – dendritic cells’ ability to activate T cells.
In healthy people, T cells play a crucial role in helping to fight infections. In people with autoimmune diseases, however, they can start to attack the body’s own tissues.
By studying cells from mice and people, the researchers found vitamin D caused dendritic cells to produce more of a molecule called CD31 on their surface and that this hindered the activation of T cells.
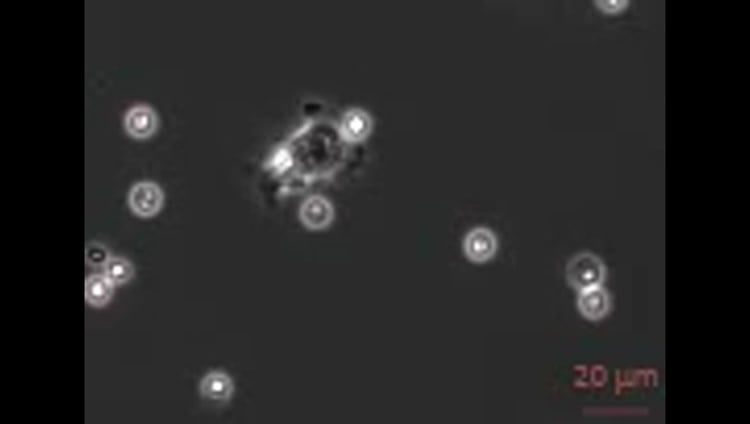
The team observed how CD31 prevented the two cell types from making a stable contact – an essential part of the activation process – and the resulting immune reaction was far reduced.
Researchers say the findings shed light on how vitamin D deficiency may regulate the immune system and influence susceptibility to autoimmune diseases.
The study, published in Frontiers in Immunology, was funded by the Medical Research Council, Biotechnology and Biological Sciences Research Council, Natural Environment Research Council and Wellcome.
Professor Richard Mellanby, of the University of Edinburgh’s Centre for Inflammation Research, said: “Low vitamin D status has long being implicated as a significant risk factor for the development of several autoimmune diseases. Our study reveals one way in which vitamin D metabolites can dramatically influence the immune system.”
Source:
University of Edinburgh
Media Contacts:
Jen Middleton – University of Edinburgh
Image Source:
The image is credited to The University of Edinburgh.
Original Research: Open access.
“1,25-Dihydroxyvitamin D3 Restrains CD4+ T Cell Priming Ability of CD11c+ Dendritic Cells by Upregulating Expression of CD31”
Louise Saul, Iris Mair, Alasdair Ivens, Pamela Brown, Kay Samuel, John D. M. Campbell, Daniel Y. Soong, Nadine Kamenjarin and Richard J. Mellanby. Frontiers in Immunology doi:10.3389/fimmu.2019.00600
Abstract
1,25-Dihydroxyvitamin D3 Restrains CD4+ T Cell Priming Ability of CD11c+ Dendritic Cells by Upregulating Expression of CD31
Dendritic cells (DC) are specialized sentinel cells that bridge the innate and adaptive immune response and play a crucial role in shaping the adaptive immune response. Vitamin D, a known epidemiological risk factor for the development of several autoimmune diseases, influences the development of dendritic cells. Consequently, vitamin D metabolites are frequently used in protocols to develop therapeutic dendritic cell therapies for autoimmune diseases. However, the mechanisms by which vitamin D modulates DC function remain poorly understood. We investigated the effects of vitamin D on murine CD11c+ bone marrow derived DC (BMDC) function by analyzing global gene expression in CD11c+ BMDC generated in the presence (VitD-CD11c+BMDC) or absence (Veh-CD11c+BMDC) of the active vitamin D metabolite, 1,25-dihydroxyvitamin D3 (1,25(OH)2D3). Seven genes were significantly increased in expression in both immature and LPS-matured VitD-CD11c+BMDC, one of which was CD31, a member of the immunoglobulin superfamily. Gene knockdown of CD31 enhanced the ability of VitD-CD11c+BMDC to prime naïve CD4+ T cells in vitro; conversely, increased expression of CD31 on vehicle treated CD11c+BMDC restrained their T cell priming abilities. Time-lapse imaging of BMDC and CD4+ T cells during in vitro priming revealed that CD31 reduced the BMDC–T cell interaction time. Finally, we confirmed a similar effect of 1,25(OH)2D3 on human CD34+ cell-derived CD11c+DC, whereby DC generated in the presence of 1,25(OH)2D3 had increased CD31 expression. In summary, we show that both mouse and human DC generated in the presence of 1,25(OH)2D3 upregulate CD31 expression, resulting in a reduced ability to prime CD4+ T cells by impairing a stable cell-cell contact.