Summary: Researchers say mental health disorders experienced earlier in life may be a salient warning for increased risks of developing dementia later in life.
Source: University of Michigan
Preventing mental disorders in young people might reduce or delay the burden of dementia in older people, according to a new study.
Investing in good mental health care for young people—including evidence-based interventions for mental health problems—could help reduce the burden of neurodegenerative disease, say researchers from the University of Michigan, Duke University and the University of Auckland.
Their study of 1.7 million New Zealanders—aged 21 to 60 years at baseline—followed across three decades (1988 to 2018) tested whether individuals with mental disorders are at increased risk for subsequent dementia.
Much research and treatment in geriatrics focuses on physical diseases and ignores mental health, says Leah Richmond-Rakerd, assistant professor in U-M’s Department of Psychology and the study’s lead author.
Richmond-Rakerd and colleagues chose New Zealand for its capacity to link medical records and other administrative databases at the population level—something not possible in the United States.
The long-term, follow-up use of hospital records, and the ability to establish that mental disorders preceded dementia set this study apart from others.
Among the study’s findings:
- Mental disorders were more strongly associated with dementia than chronic physical diseases—an outcome the researchers did not expect.
- The association between mental disorders and dementia was not explained by preexisting chronic physical illness or socioeconomic deprivation.
- The connection between mental health problems and dementia was seen for both men and women, for both early-onset and later-onset dementias, for different types of mental health conditions and for both Alzheimer’s and non-Alzheimer’s dementias.
Richmond-Rakerd says mental disorders are salient early-warning signs for subsequent dementia. People with mental disorders could be encouraged to engage in health behaviors to reduce dementia risk—for instance, to increase their physical activity, which so far is one promising way to potentially help prevent dementia, the researchers say.
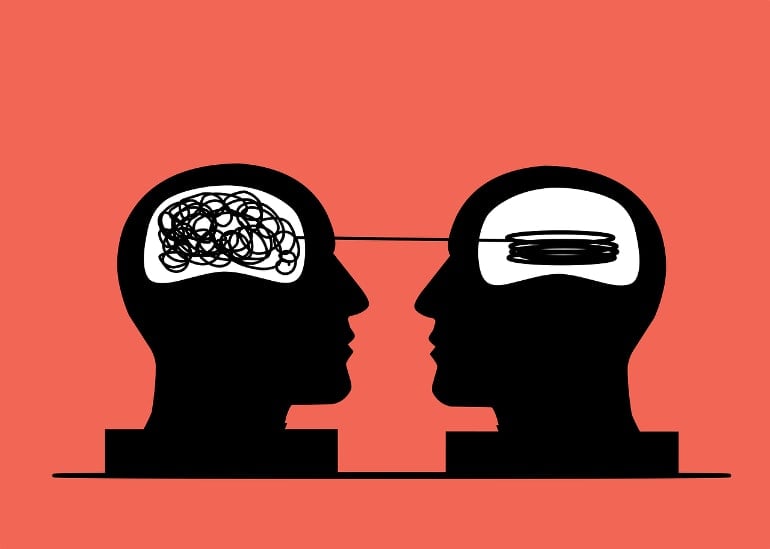
The mechanism for the association is not clear, but could involve several factors, says co-author Avshalom Caspi, professor of psychology and neuroscience at Duke.
For instance, a lifelong brain vulnerability may manifest itself as mental health problems earlier in life and dementia later in life. Or medication for mental disorders (such as antipsychotics) might increase the risk for dementia, he says.
The researchers caution that most people with mental-health problems will not develop dementia.
“Mental health problems are not a ‘life sentence’ that always results in dementia,” Richmond-Rakerd said.
About this mental health and dementia research news
Author: Jared Wadley
Source: University of Michigan
Contact: Jared Wadley – University of Michigan
Image: The image is in the public domain
Original Research: Open access.
“Longitudinal Associations of Mental Disorders With Dementia” by Leah S. Richmond-Rakerd et al. JAMA Psychiatry
Abstract
Longitudinal Associations of Mental Disorders With Dementia
Importance
Mental disorders are an underappreciated category of modifiable risk factors for dementia. Developing an evidence base about the link between mental disorders and dementia risk requires studies that use large, representative samples, consider the full range of psychiatric conditions, ascertain mental disorders from early life, use long follow-ups, and distinguish between Alzheimer disease and related dementias.
Objective
To test whether mental disorders antedate dementia across 3 decades of observation.
Design, Setting, and Participants
This population-based administrative register study of mental disorders and Alzheimer disease and related dementias included all individuals born in New Zealand between 1928 and 1967 who resided in the country for any time during the 30-year observation period between July 1988 and June 2018. Data were from the New Zealand Integrated Data Infrastructure, a collection of whole-of-population administrative data sources linked at the individual level. Data were analyzed from October 2020 to November 2021.
Exposures
Diagnoses of mental disorders were ascertained from public-hospital records.
Main Outcomes and Measures
Diagnoses of dementia were ascertained from public-hospital records, mortality records, and pharmaceutical records.
Results
Of 1 711 386 included individuals, 866 301 (50.6%) were male, and individuals were aged 21 to 60 years at baseline. Relative to individuals without a mental disorder, those with a mental disorder were at increased risk of developing subsequent dementia (relative risk [RR], 4.24; 95% CI, 4.07-4.42; hazard ratio, 6.49; 95% CI, 6.25-6.73). Among individuals with dementia, those with a mental disorder developed dementia a mean of 5.60 years (95% CI, 5.31-5.90) earlier than those without a mental disorder. Associations held across sex and age and after accounting for preexisting chronic physical diseases and socioeconomic deprivation. Associations were present across different types of mental disorders and self-harm behavior (RRs ranged from 2.93 [95% CI, 2.66-3.21] for neurotic disorders to 6.20 [95% CI, 5.67-6.78] for psychotic disorders), and were evident for Alzheimer disease (RR, 2.76; 95% CI, 2.45-3.11) and all other dementias (RR, 5.85; 95% CI, 5.58-6.13).
Conclusions and Relevance
In this study, mental disorders were associated with the onset of dementia in the population. Ameliorating mental disorders in early life might also ameliorate neurodegenerative conditions and extend quality of life in old age.