Summary: As we age, our brain naturally becomes more insulin resistant, disrupting neuron communication and leading to cognitive decline and neurodegeneration.
Researchers studied how acute insulin resistance impacts neuronal function before symptoms of chronic conditions like Alzheimer’s manifest. Using mice models, they found that ketones could restore impaired synaptic activity, axonal conduction, and network synchronization.
This research highlights potential ketone-based therapies for neurodegenerative diseases.
Key Facts:
- Acute insulin resistance in the brain impairs synaptic activity, axonal conduction, and network synchronization.
Administering ketones like D-βHb can restore these critical neuronal functions.
This research suggests new therapeutic avenues for conditions involving insulin resistance, such as diabetes and Alzheimer’s disease.
Source: University of Rochester
As we age our brain naturally becomes more insulin resistant. This creates a breakdown in communication between neurons, causing symptoms like changes in mood, cognitive decline, and eventually neurodegeneration.
Nathan A. Smith, MS, PhD (’13), associate professor of Neuroscience, and fellow researchers studied the mechanisms in the brain that break down when insulin resistance is suddenly present, like in trauma, but before symptoms manifest into chronic conditions, like diabetes or Alzheimer’s.

“Once neuronal function is lost, there is no recovering the connection, so we need to identify when the function first becomes impaired,” said Smith, the principal investigator of this research, published in the journal PNAS Nexus.
“This study accomplishes that by bringing us closer to understanding how to rescue the function of impaired neurons and prevent or delay devastating diseases like Alzheimer’s.”
Using mice as a model system, researchers focused on the hippocampus, a well understood region of the brain responsible for learning and memory. They found acute insulin resistance impairs several aspects of neuronal function, including synaptic activity, axonal conduction, network synchronization, synaptic plasticity, and action potential properties—the processes critical to support the communication flow in and out of neurons.
Researchers then administered D-βHb, a form of ketones, a byproduct released by the liver when the body burns fat instead of glucose for energy. They found that the synaptic activity that was previously impacted by acute insulin resistance was rescued, conduction in axons increased, neurons were resynchronized, and synaptic plasticity.
“This research has implications for developing ketone-based therapies targeting specific neuronal dysfunctions in conditions involving insulin resistance/hypoglycemia like diabetes or Alzheimer’s disease,” Smith said. “We are now looking to understand the role that astrocytes and other glia cells play in acute insulin resistance.”
Additional authors include Bartosz Kula, PhD, of the Del Monte Institute for Neuroscience at the University of Rochester, Botond Antal and Lilianne Mujica-Parodi, PhD, of Stony Brook University and Harvard Medical School, Corey Weistuch, PhD, of Memorial Sloan Kettering Cancer Center, Florian Gackiere, PhD, Alexander Barre, PhD, and Jeffrey Hubbard, PhD, of Neuroservices Alliance, and Maria Kukley, PhD, of Achucarro Basque Center for Neuroscience and Basque Foundation for Science.
Funding: This research was supported by The National Institutes of Health, the National Science Foundation, and the Department of Defense.
About this neurology research news
Author: Kelsie Smith Hayduk
Source: University of Rochester
Contact: Kelsie Smith Hayduk – University of Rochester
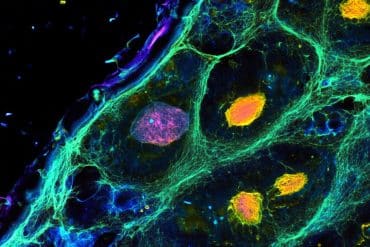
Image: The image is credited to Neuroscience News
Original Research: Open access.
“D-ꞵ-hydroxybutyrate stabilizes hippocampal CA3-CA1 circuit during acute insulin resistance” by Nathan A. Smith et al. PNAS Nexus
Abstract
D-ꞵ-hydroxybutyrate stabilizes hippocampal CA3-CA1 circuit during acute insulin resistance
The brain primarily relies on glycolysis for mitochondrial respiration but switches to alternative fuels such as ketone bodies (KBs) when less glucose is available. Neuronal KB uptake, which does not rely on glucose transporter 4 (GLUT4) or insulin, has shown promising clinical applicability in alleviating the neurological and cognitive effects of disorders with hypometabolic components.
However, the specific mechanisms by which such interventions affect neuronal functions are poorly understood. In this study, we pharmacologically blocked GLUT4 to investigate the effects of exogenous KB D-ꞵ-hydroxybutyrate (D-ꞵHb) on mouse brain metabolism during acute insulin resistance (AIR).
We found that both AIR and D-ꞵHb had distinct impacts across neuronal compartments: AIR decreased synaptic activity and long-term potentiation (LTP) and impaired axonal conduction, synchronization, and action potential properties, while D-ꞵHb rescued neuronal functions associated with axonal conduction, synchronization, and LTP.