Summary: Research suggests a high-sugar diet, commonly associated with obesity, leads to insulin resistance in the brain and may heighten the risk of neurodegenerative diseases like Alzheimer’s.
The study reveals that this insulin resistance impairs glial cells’ ability to clear neuronal debris, a crucial process for preventing neurodegeneration.
By studying fruit flies, which share physiological similarities with humans, the team uncovered that a sugar-rich diet decreases the levels of the PI3k protein in glial cells and Draper protein in ensheathing glia, hindering their debris-clearing functions.
Key Facts:
- Obesity-related high-sugar diets can cause insulin resistance in the brain, which was demonstrated to reduce the brain’s capacity to remove neuronal debris.
- The study found that this resistance lowers PI3k and Draper protein levels in glial cells, directly impacting their debris-clearing abilities.
- These findings connect diet-induced insulin resistance to an increased risk of neurodegenerative diseases, offering new insights for preventive therapies.
Source: PLOS
Researchers led by Mroj Alassaf at the Fred Hutchinson Cancer Research Center in the United States have discovered a link between obesity and neurodegenerative disorders like Alzheimer’s disease.
Using the common fruit fly, the research shows that a high-sugar diet — a hallmark of obesity — causes insulin resistance in the brain, which in turn reduces the ability to remove neuronal debris, thus increasing the risk of neurodegeneration.
Publishing November 7th in the open access journal PLOS Biology, the research will impact therapies designed to reduce the risk of developing neurodegenerative diseases.
Although obesity is known to be a risk factor for neurodegenerative disorders like Alzheimer’s disease and Parkinson’s disease, exactly how one leads to the other remains a mystery. The new study focused on answering this question by taking advantage of the similarity between humans and fruit flies.
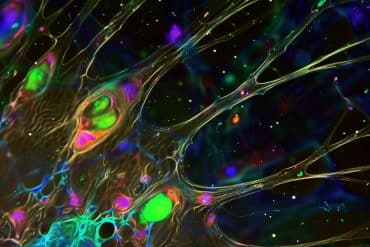
Having previously shown that a high-sugar diet leads to insulin resistance in the peripheral organs of flies, the researchers now turned to their brains. Specifically, they examined glial cells because microglial dysfunction is known to lead to neural degeneration.
Levels of the protein PI3k indicate how much a cell is able to respond to insulin. The researchers found that the high sugar diet led to reduced PI3k levels in glial cells, indicating insulin resistance.
They also looked at the fly equivalent of microglia, called ensheathing glia, whose primary function is to remove neural debris, such as degenerating axons. They observed that these glia had low levels of the protein Draper, indicating impaired function.
Further tests revealed that artificial reduction of PI3k levels led to both insulin resistance and low Draper levels in ensheathing glia.
Finally, they showed that after actually damaging olfactory neurons, the ensheathing glia could not remove the degenerating axons in the flies on the high sugar diet because their Draper levels did not increase.
The authors add, “Using fruit flies, the authors establish that high-sugar diets trigger insulin resistance in glia, disrupting their ability to clear neuronal debris. This study provides insight into how obesity-inducing diets potentially contribute to the increased risk of neurodegenerative disorders.”
About this diet, obesity, and neurodegeneration research news
Author: Claire Turner
Source: PLOS
Contact: Claire Turner – PLOS
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Diet-induced glial insulin resistance impairs the clearance of neuronal debris in Drosophila brain” by Akhila Rajan et al. PLOS Biology
Abstract
Diet-induced glial insulin resistance impairs the clearance of neuronal debris in Drosophila brain
Obesity significantly increases the risk of developing neurodegenerative disorders, yet the precise mechanisms underlying this connection remain unclear. Defects in glial phagocytic function are a key feature of neurodegenerative disorders, as delayed clearance of neuronal debris can result in inflammation, neuronal death, and poor nervous system recovery.
Mounting evidence indicates that glial function can affect feeding behavior, weight, and systemic metabolism, suggesting that diet may play a role in regulating glial function. While it is appreciated that glial cells are insulin sensitive, whether obesogenic diets can induce glial insulin resistance and thereby impair glial phagocytic function remains unknown.
Here, using a Drosophila model, we show that a chronic obesogenic diet induces glial insulin resistance and impairs the clearance of neuronal debris. Specifically, obesogenic diet exposure down-regulates the basal and injury-induced expression of the glia-associated phagocytic receptor, Draper.
Constitutive activation of systemic insulin release from Drosophila insulin-producing cells (IPCs) mimics the effect of diet-induced obesity on glial Draper expression. In contrast, genetically attenuating systemic insulin release from the IPCs rescues diet-induced glial insulin resistance and Draper expression.
Significantly, we show that genetically stimulating phosphoinositide 3-kinase (Pi3k), a downstream effector of insulin receptor (IR) signaling, rescues high-sugar diet (HSD)-induced glial defects.
Hence, we establish that obesogenic diets impair glial phagocytic function and delays the clearance of neuronal debris.