Summary: Researchers discuss the need for long-term and more quantitative approaches by experts spanning various fields, to help understand viruses, like SARS-CoV-2, and how they may affect drinking water treatment strategies.
Source: Stanford University
Engineers at Stanford describe potential transmission pathways of COVID-19 and their implications.
Much remains unknown about how SARS-CoV-2, the virus that causes COVID-19, spreads through the environment. A major reason for this is that the behaviors and traits of viruses are highly variable – some spread more easily through water, others through air; some are wrapped in layers of fatty molecules that help them avoid their host’s immune system, while others are “naked.”
This makes it urgent for environmental engineers and scientists to collaborate on pinpointing viral and environmental characteristics that affect transmission via surfaces, the air and fecal matter, according to Alexandria Boehm, a Stanford professor of civil and environmental engineering, and Krista Wigginton, the Shimizu Visiting Professor in Stanford’s department of civil and environmental engineering and an associate professor at the University of Michigan.
Boehm and Wigginton co-authored a recently published viewpoint in Environmental Science & Technology calling for a broader, long-term and more quantitative approach to understanding viruses, such as SARS-CoV-2, that are spread through the environment. They are also principal investigators on a recently announced National Science Foundation-funded project to study the transfer of coronaviruses between skin and other materials, the effect of UV and sunlight on the coronaviruses, and the connection between disease outbreaks and virus concentrations in wastewater.
Scientists and medical experts don’t have a good understanding of what virus characteristics and environmental factors control virus persistence in the environment – for example, in aerosols and droplets, on surfaces including skin and in water including seawater, according to Boehm and Wigginton. “When a new virus emerges and poses a risk to human health, we don’t have a good way of predicting how it will behave in the environment,” Boehm said.
Part of the problem is historically there has been limited funding for this sort of work. The National Institutes of Health historically hasn’t funded work on pathogens in the environment, and funding at the National Science Foundation for this work is limited. Also, coronaviruses and most of the emerging viruses that have caught the world’s attention over the last decade are enveloped viruses that are wrapped in an outer layer of fatty lipid molecules that they’ve stolen from their hosts. Proteins on the surface of the envelopes can help these viruses evade the immune systems of the organisms they are infecting. “There has been much more work on the fate of non-enveloped or naked viruses because most intestinal pathogens in excrement are nonenveloped viruses – like norovirus and rotavirus,” said Wigginton.
In their paper, Boem and Wigginton address potential threats that viruses such as SARS-CoV-2 pose to water sources. We usually only worry about viruses in water if they are excreted by humans in their feces and urine. Most enveloped viruses aren’t excreted in feces or urine, so they aren’t usually on our minds when it comes to our water sources. There is increasing evidence that the SARS-CoV-2 viruses, or at least their genomes, are excreted in feces. If infective viruses are excreted, then fecal exposure could be a route of transmission, according to Boehm, who added, “It’s unlikely this could be a major transmission route, but a person could potentially be exposed by interacting with water contaminated with untreated fecal matter.”
Drinking water treatment systems have numerous treatment barriers to remove the most prevalent viruses and the most difficult-to-remove viruses, according to the engineers. Research on viruses similar to the SARS-CoV-2 virus suggests they are susceptible to these treatments. “In terms of virus concentration and persistence, this isn’t a worst-case scenario,” Wigginton said.
Broadly, Wigginton and Boehm write, we tend to study viruses very intensely when there is an outbreak, but the results from one virus aren’t easy to extrapolate to other viruses that emerge years later. “If we took a broader approach to studying many kinds of viruses, we could better understand the characteristics driving their environmental fate,” Wigginton said.
The two researchers call for experts across various fields – including medicine and engineering and – to work together to move methods forward faster, make discoveries and formulate strategies that wouldn’t be possible independently.
Source:
Stanford University
Article by Rob Jordan
Media Contact:
Rob Jordan
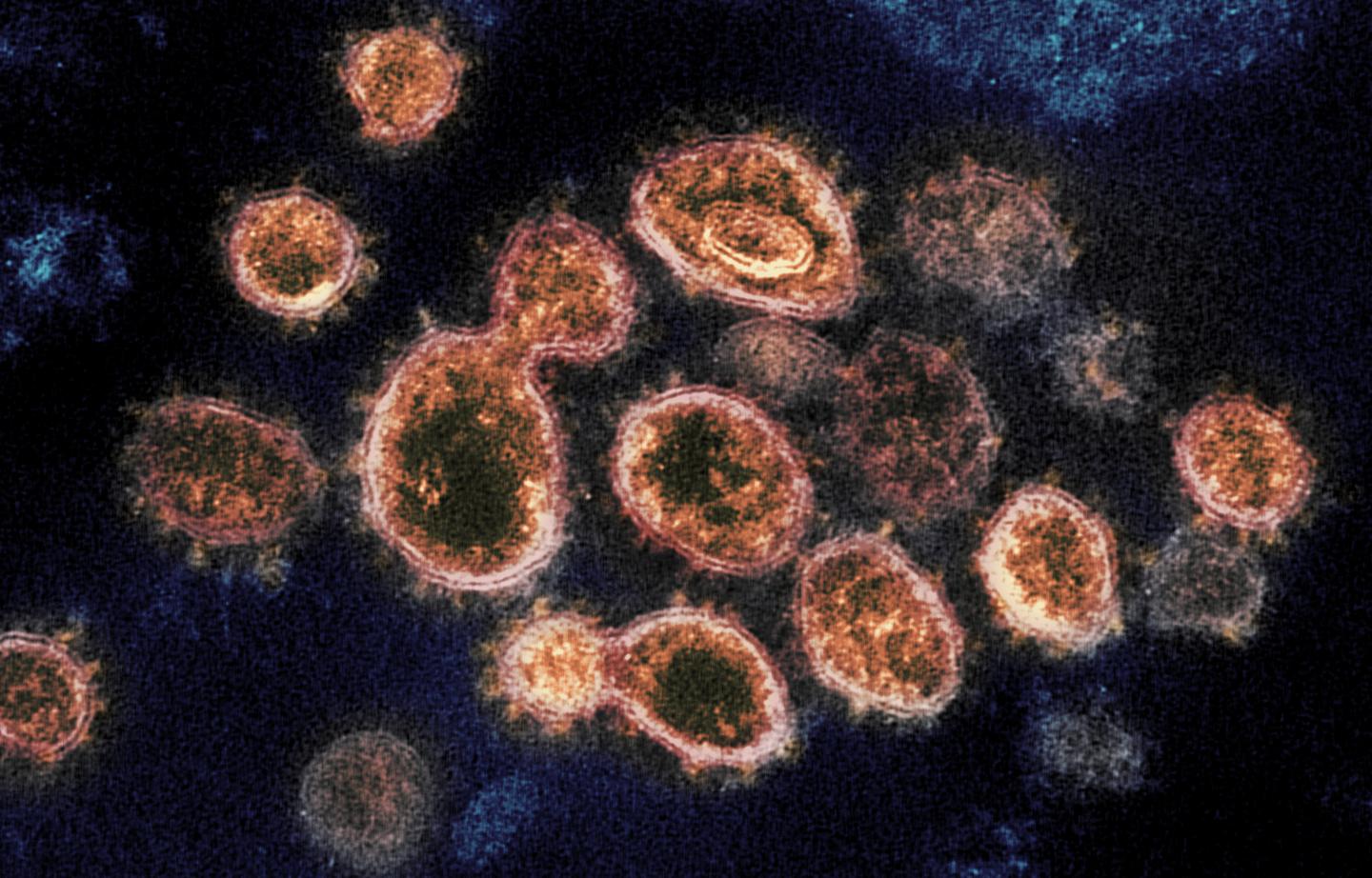
Image: This transmission electron microscope image shows SARS-CoV-2, the virus that causes COVID-19. Credit: NIAID-RML
Original Research: Opinion
“Environmental Engineers and Scientists Have Important Roles to Play in Stemming Outbreaks and Pandemics Caused by Enveloped Viruses” by Krista R. Wigginton and Alexandria B. Boehm
March 24, 2020 in Environmental Science and Technology
doi.org/10.1021/acs.est.0c01476