Summary: Researchers identified a new form of cell death, termed ferroptosis, in Alzheimer’s disease and vascular dementia. This process involves the destruction of microglia cells—brain immune cells—due to the accumulation of iron.
The findings emerged when researchers analyzed post-mortem brain tissues of dementia patients, revealing that microglia were destroyed while attempting to clear iron-rich myelin. This new insight into microglial degeneration could revolutionize therapeutic approaches for these neurodegenerative diseases.
Key Facts:
- For the first time, scientists found that ferroptosis—cell death caused by iron accumulation—destroys microglia cells in Alzheimer’s and vascular dementia.
- Microglia, the brain’s immune cells, die while clearing iron-rich myelin, a previously unrecognized aspect of dementia.
- The research suggests a pivotal role of microglial degeneration in the progression of cognitive decline in dementia, potentially leading to novel therapeutic interventions.
Source: Oregon Health and Science University
Researchers have discovered a new avenue of cell death in Alzheimer’s disease and vascular dementia.
A new study, led by scientists at Oregon Health & Science University and published online in the journal Annals of Neurology on Aug. 21, reveals for the first time that a form of cell death known as ferroptosis — caused by a buildup of iron in cells — destroys microglia cells, a type of cell involved in the brain’s immune response, in cases of Alzheimer’s and vascular dementia.
The researchers conducted the study examining post-mortem human brain tissue of patients with dementia.
“This is a major finding,” said senior author Stephen Back, M.D., Ph.D., a neuroscientist and professor of pediatrics in the OHSU School of Medicine.
Back has long studied myelin, the insulation-like protective sheath covering nerve fibers in the brain, including delays in forming myelin in premature infants. The new research extends that line of work by uncovering a cascading form of neurodegeneration triggered by deterioration of myelin.
They made the discovery using a novel technique developed by the study’s lead author Philip Adeniyi, Ph.D., a postdoctoral researcher in Back’s laboratory.
The researchers discovered that microglia degenerates in the white matter of the brain of patients with Alzheimer’s and vascular dementia.
Microglia are resident cells in the brain normally involved in clearing cellular debris as part of the body’s immune system. When myelin is damaged, microglia swarm in to clear the debris. In the new study, researchers found that microglia themselves are destroyed by the act of clearing iron-rich myelin — a form of cell death known as ferroptosis.
Given the intense scientific focus on the underlying cause of dementia in older adults, Back called it amazing that researchers hadn’t made the connection to ferroptosis until now.
“We’ve missed a major form of cell death in Alzheimer’s disease and vascular dementia,” Back said. “We hadn’t been giving much attention to microglia as vulnerable cells, and white matter injury in the brain has received relatively little attention.”
Co-author Kiera Degener-O’Brien, M.D., initially discovered the degeneration of microglia in tissue samples, Back said. Adeniyi subsequently developed a novel immunofluorescence technique to determine that iron toxicity was causing microglial degeneration in the brain. This was likely a result of the fact that the fragments of myelin are themselves rich in iron, Back said.
In effect, the immune cells were dying in the line of duty.
“Everyone knows that microglia are activated to mediate inflammation,” Back said. “But no one knew that they were dying in such large numbers. It’s just amazing that we missed this until now.”
The study finds that the cascading effect of degenerating microglia appears to be a mechanism in advancing cognitive decline in Alzheimer’s disease and vascular dementia, Back said. He expects pharmaceutical companies will use this new finding to develop compounds focused on reducing microglial degeneration in the brain.
“That’s where the field will go next,” he said. “A discovery like ours will stimulate a lot of excitement in the pharmaceutical industry to develop therapeutically important compounds.”
He said the underlying cause initiating the cycle of decline likely relates to repeated episodes of low blood flow and oxygen delivery to the brain over time due to acute stroke or chronic conditions such as hypertension and diabetes.
“Dementia is a process that goes on for years and years,” Back said. “We have to tackle this from the early days to have an impact so that it doesn’t spin out of control.”
Funding: The research was supported by grants from the National Institute on Aging (AG065406, AG031892, U01 AG006781, and U19 AG066567 which supports the ACT study, p50 AG005136 and p30AG066509, which support the UW Alzheimer’s disease Research Center) of the National Institutes of Health; the National Institute of Neurological Disorders and Stroke of the NIH (NS105984); and by the Nancy and Buster Alvord Endowment. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
About this Alzheimer’s disease research news
Author: Erik Robinson
Source: Oregon Health and Science University
Contact: Erik Robinson – Oregon Health and Science University
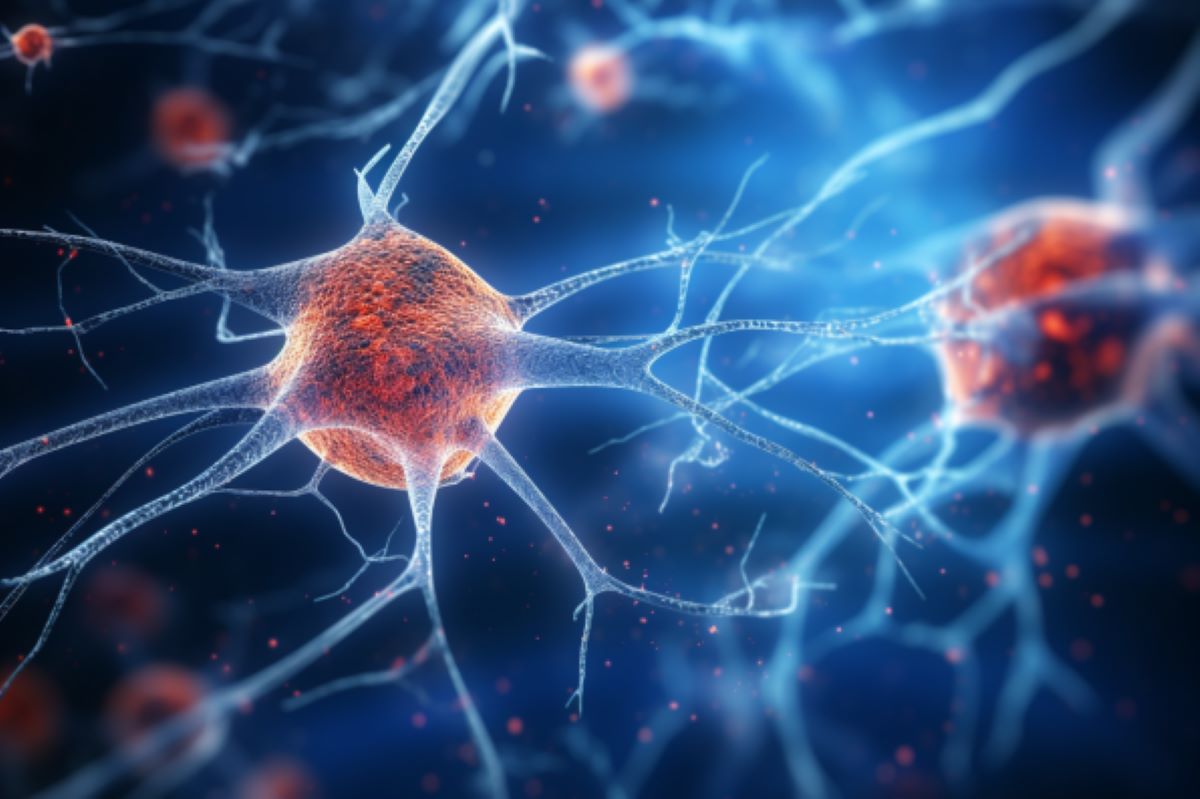
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Ferroptosis of microglia in aging human white matter injury” by Stephen Back et al. Annals of Neurology
Abstract
Ferroptosis of microglia in aging human white matter injury
Objective
Since the role of white matter (WM) degenerating microglia in myelination failure is unclear, we sought to define the core features of this novel population of aging human microglia.
Methods
We analyzed post-mortem human brain tissue to define a population of degenerative microglia (DM) in aging white matter lesions. We employed immunofluorescence staining and gene expression analysis to investigate molecular mechanisms related to the degeneration of DM.
Results
We found that DM accumulated myelin debris, were selectively enriched in the iron-binding protein light chain ferritin, and accumulated PLIN2-labeled lipid droplets. DM displayed lipid peroxidation injury and enhanced expression for TOM20, a mitochondrial translocase, and a sensor of oxidative stress. DM also displayed enhanced expression of the DNA fragmentation marker phospho-histone H2A.X. We identified a unique set of ferroptosis-related genes involving iron-mediated lipid dysmetabolism and oxidative stress that were preferentially expressed in white matter injury relative to gray matter neurodegeneration.
Interpretation
Ferroptosis appears to be a major mechanism of white matter injury in Alzheimer’s disease and vascular dementia. White matter DM are a novel therapeutic target to potentially reduce the impact of white matter injury and myelin loss on the progression of cognitive impairment.







