Summary: Using EEG to measure electrical activity in the brain can help doctors predict a patient’s response to antidepressants, a new study reveals.
Source: UT Southwestern.
Imagine millions of depressed Americans getting their brain activity measured and undergoing blood tests to determine which antidepressant would work best. Imagine some of them receiving “brain training” or magnetic stimulation to make their brains more amenable to those treatments.
A national research trial initiated by UT Southwestern in 2012 is generating the first set of results this year that provides an early glimpse into how such high-tech strategies may change the field of mental health.
The first study – to be published in the June edition of the Journal of the American Medical Association Psychiatry – found that measuring electrical activity in the brain can help predict a patient’s response to an antidepressant. In the coming months, at least four more studies evaluating the effectiveness of other predictive tests are expected to derive from the EMBARC trial, a major thrust of a national effort to establish biology-based, objective strategies to remedy mood disorders.
“When the results from these tests are combined, we hope to have up to 80 percent accuracy in predicting whether common antidepressants will work for a patient. This research is very likely to alter the mindset of how depression should be diagnosed and treated,” said Dr. Madhukar Trivedi, who oversees EMBARC and is founding Director of UT Southwestern’s Center for Depression Research and Clinical Care, a cornerstone of the Peter O’Donnell Jr. Brain Institute.
Finding solutions
Dr. Trivedi organized EMBARC with several other academic centers after the world’s largest depression study that he led more than a decade ago detailed shortcomings in patient care. Among other major findings, the STAR*D studies found that up to two-thirds of patients do not adequately respond to their first antidepressant.
Dr. Trivedi sought to improve this situation by spearheading the 16-week EMBARC trial at four U.S. sites in which more than 300 patients with major depressive disorder were evaluated through brain imaging and various DNA, blood, and other tests.
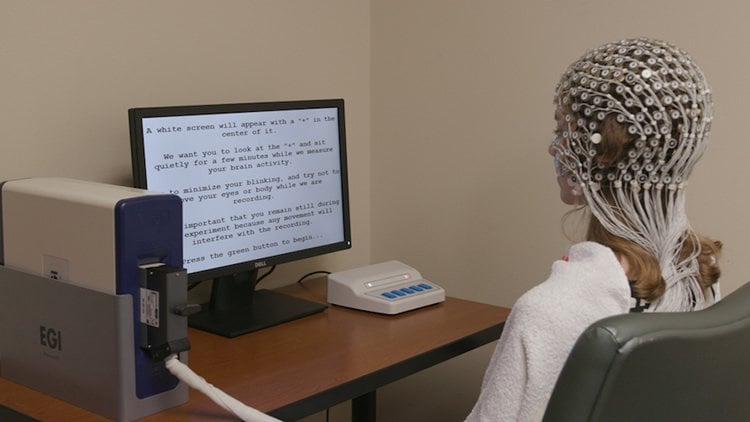
The project’s first published study focuses on how electrical activity in the brain can indicate whether a patient is likely to benefit from an SSRI (selective serotonin reuptake inhibitor), the most common class of antidepressant. Researchers used an electroencephalogram, or EEG, a noninvasive test that measured activity in the brain’s rostral anterior cingulate cortex. Patients with higher activity were more likely to respond to the SSRI within about two months.
Dr. Trivedi said EEGs have the potential to be used in combination with brain imaging and blood tests to help patients who don’t respond to SSRIs find effective treatments more quickly. He also suggested that more studies may yield useful methods to boost neural activity and make the brain more responsive to SSRIs – perhaps either through psychotherapy or magnetic stimulation on the cortex.
“Like STAR*D, I expect these studies will have a widespread effect on how we design and plan treatment approaches,” Dr. Trivedi said. “My goal is to establish blood tests and brain imaging as standard strategies in the treatment of depression.”
Benchmark research
Dr. Trivedi’s work is becoming increasingly critical in the U.S. as the depression rate continues to soar. According to data from the National Health and Nutrition Examination Survey, more than 34 million adults took antidepressants in 2013-14 – more than double the number in the 1999-2000 survey.
Some depressed patients have been diagnosed with other mood disorders such as schizophrenia or bipolar disorder – conditions that have also lacked biological markers and objective treatment strategies. UT Southwestern faculty have received national accolades for helping the field progress in this area. The recognitions include receiving the American Psychiatric Association’s top research award for two consecutive years, largely for STAR*D and for creating a new system of classifying various forms of psychosis based on biological indicators.
Understanding mood disorders
Meanwhile, Dr. Trivedi has initiated other large research projects to further understand the underpinnings of mood disorders, among them D2K, a study that will enroll 2,000 patients with depression and bipolar disorders and follow them for 20 years. In addition, RAD is a 10-year study of 1,500 participants (ages 10-24) that will uncover factors that reduce the risk of developing mood or anxiety disorders.
Utilizing some of these enrollees, Dr. Trivedi’s research team will study the results from a battery of other tests to augment EEGs and more accurately assess patients’ biological signatures and determine the most effective treatment. Dr. Trivedi has had preliminary success developing a blood test but acknowledges it may only benefit patients with a specific type of inflammation.
Combining blood and brain tests, he said, will improve the chances of choosing the right treatment the first time.
“Although we continue to study brain imaging and blood biomarkers, I do recommend patients ask for these tests when seeking an antidepressant,” Dr. Trivedi said. “Your performance on them, when appropriate, will tell you to try this or avoid that. The bottom line is to reduce the trial-and-error process that can be so devastating to patients.”
Dr. Trivedi is a Professor of Psychiatry who holds the Betty Jo Hay Distinguished Chair in Mental Health and the Julie K. Hersh Chair for Depression Research and Clinical Care. Funded by the National Institute of Mental Health, EMBARC (Establishing Moderators and Biosignatures of Antidepressant Response for Clinical Care) was a multicenter effort that also involved researchers at Harvard Medical School and Massachusetts General Hospital, Columbia University, McLean Hospital, Stanford University, University of Pittsburgh, and the University of Michigan.
Source: James Beltran – UT Southwestern
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to UT Southwestern.
Original Research: Abstract for “Pretreatment Rostral Anterior Cingulate Cortex Theta Activity in Relation to Symptom Improvement in Depression: A Randomized Clinical Trial” by Diego A. Pizzagalli, PhD; Christian A. Webb, PhD; Daniel G. Dillon, PhD; Craig E. Tenke, PhD; Jürgen Kayser, PhD; Franziska Goer, MA; Maurizio Fava, MD; Patrick McGrath, MD; Myrna Weissman, PhD; Ramin Parsey, MD, PhD; Phil Adams, PhD; Joseph Trombello, PhD; Crystal Cooper, PhD; Patricia Deldin, PhD; Maria A. Oquendo, MD, PhD; Melvin G. McInnis, MD; Thomas Carmody, PhD; Gerard Bruder, PhD; and Madhukar H. Trivedi, MD in JAMA Psychiatry. Published April 11 2018.
doi:10.1001/jamapsychiatry.2018.0252
[cbtabs][cbtab title=”MLA”]UT Southwestern “EEG Brain Test Helps Patients Overcome Depression.” NeuroscienceNews. NeuroscienceNews, 16 May 2018.
<https://neurosciencenews.com/eeg-depression-9068/>.[/cbtab][cbtab title=”APA”]UT Southwestern (2018, May 16). EEG Brain Test Helps Patients Overcome Depression. NeuroscienceNews. Retrieved May 16, 2018 from https://neurosciencenews.com/eeg-depression-9068/[/cbtab][cbtab title=”Chicago”]UT Southwestern “EEG Brain Test Helps Patients Overcome Depression.” https://neurosciencenews.com/eeg-depression-9068/ (accessed May 16, 2018).[/cbtab][/cbtabs]
Abstract
Pretreatment Rostral Anterior Cingulate Cortex Theta Activity in Relation to Symptom Improvement in Depression: A Randomized Clinical Trial
Importance Major depressive disorder (MDD) remains challenging to treat. Although several clinical and demographic variables have been found to predict poor antidepressant response, these markers have not been robustly replicated to warrant implementation in clinical care. Increased pretreatment rostral anterior cingulate cortex (rACC) theta activity has been linked to better antidepressant outcomes. However, no prior study has evaluated whether this marker has incremental predictive validity over clinical and demographic measures.
Objective To determine whether increased pretreatment rACC theta activity would predict symptom improvement regardless of randomization arm.
Design, Setting, and Participants A multicenter randomized clinical trial enrolled outpatients without psychosis and with chronic or recurrent MDD between July 29, 2011, and December 15, 2015 (Establishing Moderators and Biosignatures of Antidepressant Response for Clinical Care [EMBARC]). Patients were consecutively recruited from 4 university hospitals: 634 patients were screened, 296 were randomized to receive sertraline hydrochloride or placebo, 266 had electroencephalographic (EEG) recordings, and 248 had usable EEG data. Resting EEG data were recorded at baseline and 1 week after trial onset, and rACC theta activity was extracted using source localization. Intent-to-treat analysis was conducted. Data analysis was performed from October 7, 2016, to January 19, 2018.
Interventions An 8-week course of sertraline or placebo.
Main Outcomes and Measures The 17-item Hamilton Rating Scale for Depression score (assessed at baseline and weeks 1, 2, 3, 4, 6, and 8).
Results The 248 participants (160 [64.5%] women, 88 [35.5%] men) with usable EEG data had a mean (SD) age of 36.75 (13.15) years. Higher rACC theta activity at both baseline (b = −1.05; 95% CI, −1.77 to −0.34; P = .004) and week 1 (b = −0.83; 95% CI, −1.60 to −0.06; P < .04) predicted greater depressive symptom improvement, even when controlling for clinical and demographic variables previously linked with treatment outcome. These effects were not moderated by treatment arm. The rACC theta marker, in combination with clinical and demographic variables, accounted for an estimated 39.6% of the variance in symptom change (with 8.5% of the variance uniquely attributable to the rACC theta marker). Conclusions and Relevance Increased pretreatment rACC theta activity represents a nonspecific prognostic marker of treatment outcome. This is the first study to date to demonstrate that rACC theta activity has incremental predictive validity. Trial Registration clinicaltrials.gov Identifier: NCT01407094