Summary: Organ-on-a-chip models reveal how different tissue contribute to inflammatory diseases such as ulcerative colitis.
Source: MIT
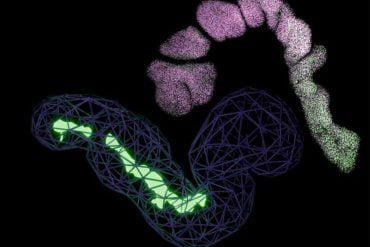
MIT biological engineers have created a multi-tissue model that lets them study the relationships between different organs and the immune system, on a specialized microfluidic platform seeded with human cells.
Using this type of model, sometimes called “organs-on-a-chip” or “physiome on-a-chip,” the research team was able to explore the role of circulating immune cells in ulcerative colitis and other inflammatory diseases. They also discovered that a metabolic byproduct generated by bacteria living in the human gut plays an important role under these inflammatory conditions.
“We’ve shown that now you can start to attack some of these really thorny, chronic inflammatory diseases by designing experiments in these organs on chips,” says Linda Griffith, the School of Engineering Professor of Teaching Innovation, a professor of biological engineering and mechanical engineering, and the senior author of the study.
This approach, described today in the journal Cell Systems, could also lend itself to studying many other complex diseases, the researchers say.
“Now we have options to really decrease or increase the level of disease complexity, under controlled and systematic conditions,” says Martin Trapecar, an MIT postdoc and the lead author of the paper.
Complex models
Nearly 20 years ago, Griffith’s lab first began working on a model of the human liver known as the “liver chip.” This system, which consists of engineered human liver tissue grown on a specialized scaffold, can be used to test drug toxicity. More recently, she has been working on small-scale replicas of many interconnected organs, also known as microphysiological systems (MPS). In 2018, she reported the development of a platform that could be used to model interactions between up to 10 organs at a time.
These kinds of devices are well-suited for analyzing complex diseases, including those that involve multiple organs, are influenced by the immune system, or cannot be accounted for by a single gene or small number of genes.
“We wanted to build technologies that would let you connect several organ systems together, so that we could start to develop new tools to combat chronic inflammatory diseases,” Griffith says. “In drug development, the field really struggles with anything that’s not a single-gene disease.”
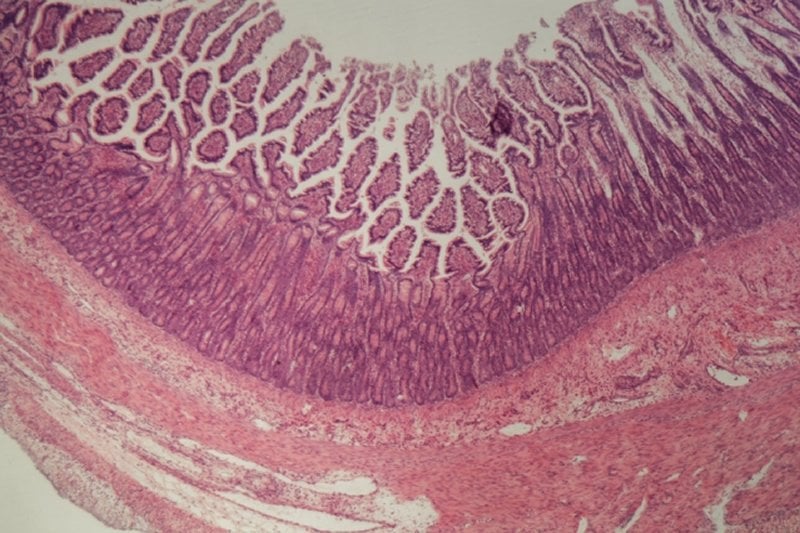
In the new Cell Systems study, she and Trapecar set out to model interactions between two organs, the colon and the liver. They also wanted to study how the immune system, especially T cells, influences those organs. It is already known that up to 80 percent of patients with a chronic liver autoimmune disease called primary sclerosing cholangitis also suffer from inflammatory bowel disease (IBD). And, patients with IBD have a much greater chance of developing autoimmune disorders of the liver.
The new system contains colon cells taken from patients with ulcerative colitis, along with healthy liver cells. The researchers found that when these tissues were connected, their physiological behavior completely changed as compared to when they are isolated. Inflammation in ulcerative colitis gut tissue decreased when the tissue was exposed to healthy liver cells. At the same time, genes and cellular pathways involved in metabolism and immune function became more active in both organs.
The researchers then added two types of T cells to the system: CD4+ T regulatory cells, which suppress other immune cells, and TH17 cells, which stimulate inflammation. Adding these T cells to the gut-liver interaction quickly increased inflammation and recreated certain features of both IBD and autoimmune liver diseases.
Lastly, the researchers decided to investigate the potential role of molecules called short-chain fatty acids (SCFAs) in inflammatory disease. These molecules are produced by microbes in the human gut as they feast on undigested fiber. SCFAs, which include butyrate, propionate, and acetate, are produced in large quantities and account for about 10 percent of our daily energy needs.
While these compounds have many beneficial effects in the human body, including reducing inflammation, a few studies in recent years have suggested that SCFAs can also cause harm by stimulating inflammation. The new MIT study found that adding SCFAs to the ulcerative colitis model greatly exacerbated inflammation throughout the liver and gut, but only if T cells were already present.
“The hypothesis we formed, based on these studies, is that the role of short chain fatty acids seems to depend on how much the adaptive immune system (which includes T cells) is involved,” Trapecar says.
That is, in early stages of inflammation, when T cells are not heavily involved, SCFAs can help reduce inflammation. But when many effector T cells are recruited, SCFAs stimulate them to be even more inflammatory. This could be useful in cases of infection, to help the body to fend off invaders, but it can also accelerate autoimmune disorders.
Modeling brain disorders
This study grew out of a related project in which the researchers planned to look at interactions between the gut, liver, and brain. A recent study from Sarkis Mazmanian, a professor of microbiology at Caltech, showed that in a mouse model of Parkinson’s, germ-free mice developed signs of the disease later than those housed under regular conditions. The study suggested that SCFAs produced by microbes might contribute to the observed phenomena and progression of the disease.
Griffith’s lab is now working to use the MPS system to shed light on the connection between SCFAs and Parkinson’s disease. The researchers also plan to study other complex diseases, in hopes that their results will help guide the development of new treatments for disorders that are currently difficult to treat.
“You really need very complex models,” Griffith says. “You can certainly get hypotheses from animal models, but to really go forward in drug development, you need better ways to identify targets that build on samples from human patients.”
Funding: The research was funded by the U.S. Defense Advanced Research Projects Agency, the National Institutes of Health, the National Institute of Biomedical Imaging and Bioengineering, the National Institute of Environmental Health Sciences, the Koch Institute Support (core) Grant from the National Cancer Institute, and the Pew-Stewart Trust Foundation.
Source:
MIT
Media Contacts:
Anne Trafton – MIT
Image Source:
The image is credited to Linda Griffith et al.
Original Research: Closed access
“Gut-Liver Physiomimetics Reveal Paradoxical Modulation of IBD-Related Inflammation by Short-Chain Fatty Acids”. Martin Trapecar, Catherine Communal, Jason Velazquez, Christian Alexander Maass, Yu-Ja Huang, Kirsten Schneider, Charles W. Wright, Vincent Butty, and others.
Cell Systems doi:10.1016/j.cels.2020.02.008.
Abstract
Gut-Liver Physiomimetics Reveal Paradoxical Modulation of IBD-Related Inflammation by Short-Chain Fatty Acids
Highlights
• We developed a model of the human gut-liver axis, including adaptive immune cells
• Interaction between gut and liver MPSs increases metabolism and reduces inflammation
• SCFAs reduce innate inflammation of the UC gut in absence of Treg and Th17 cells
• Acute CD4 + T cell-mediated inflammation is exacerbated by SCFAs
Summary
Although the association between the microbiome and IBD and liver diseases is known, the cause and effect remain elusive. By connecting human microphysiological systems of the gut, liver, and circulating Treg and Th17 cells, we created a multi-organ model of ulcerative colitis (UC) ex vivo. The approach shows microbiome-derived short-chain fatty acids (SCFAs) to either improve or worsen UC severity, depending on the involvement of effector CD4 T cells. Using multiomics, we found SCFAs increased production of ketone bodies, glycolysis, and lipogenesis, while markedly reducing innate immune activation of the UC gut. However, during acute T cell-mediated inflammation, SCFAs exacerbated CD4 + T cell-effector function, partially through metabolic reprograming, leading to gut barrier disruption and hepatic injury. These paradoxical findings underscore the emerging utility of human physiomimetic technology in combination with systems immunology to study causality and the fundamental entanglement of immunity, metabolism, and tissue homeostasis.