Summary: New studies find a drug designed to combat the gene that causes SCA2 could also be beneficial in the fight against ALS.
Source: UT Southwestern.
Using the new gene-editing enzyme CRISPR-Cpf1, researchers at UT Southwestern Medical Center have successfully corrected Duchenne muscular dystrophy in human cells and mice in the lab.
The UT Southwestern group had previously used CRISPR-Cas9, the original gene-editing system, to correct the Duchenne defect in a mouse model of the disease and in human cells. In the current work, they used a new variation of the gene-editing system to repair the defect in both a mouse model and in human cells.
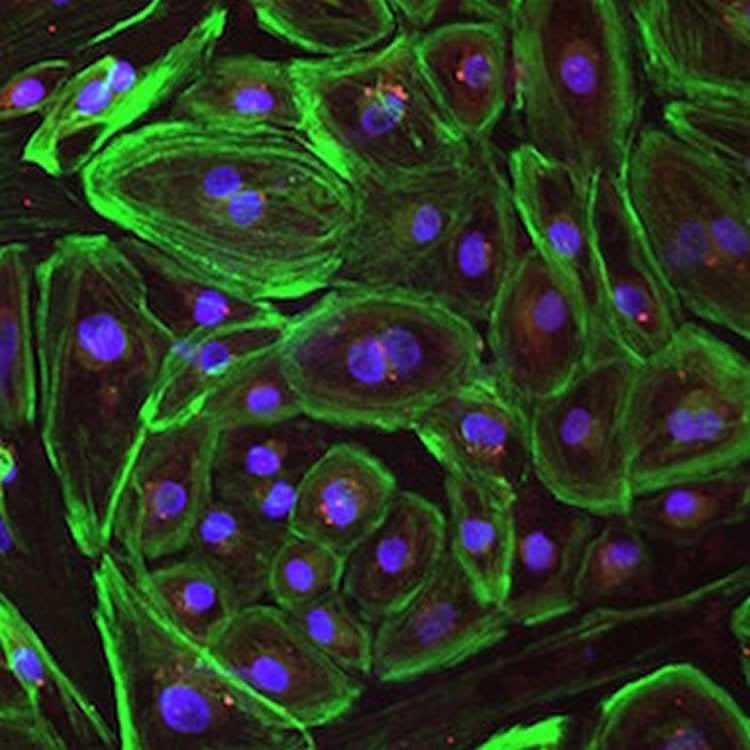
“We took patient-derived cells that had the most common mutation responsible for Duchenne muscular dystrophy and we corrected them in vitro to restore production of the missing dystrophin protein in the cells. This work provides us with a promising new tool in the CRISPR toolbox,” said author Dr. Eric Olson, Chairman of Molecular Biology, Co-Director of the UT Southwestern Wellstone Muscular Dystrophy Cooperative Research Center, and Director of the Hamon Center for Regenerative Science and Medicine.
The research appears in the journal Science Advances.
CRISPR-Cpf1 differs from CRISPR-Cas9 in a number of key ways. Cpf1 is much smaller than the Cas9 enzyme, which makes it easier to package inside a virus and therefore easier to deliver to muscle cells.
It also recognizes a different sequence of DNA than Cas9 does, which provides greater flexibility in terms of use. “There will be some genes that may be difficult to edit with Cas9 but may be easier to modify with Cpf1, or vice versa. The two proteins have different biochemical properties and recognize different DNA sequences, so these properties create more options for gene-editing,” said Dr. Olson, who holds the Pogue Distinguished Chair in Research on Cardiac Birth Defects, the Robert A. Welch Distinguished Chair in Science, and the Annie and Willie Nelson Professorship in Stem Cell Research.
“By either skipping a mutation region or precisely repairing a mutation in the gene, CRISPR-Cpf1-mediated genome editing not only corrects Duchenne muscular dystrophy mutations but also improves muscle contractility and strength,” said co-author Dr. Rhonda Bassel-Duby, Professor of Molecular Biology and Associate Director of the Hamon Center for Regenerative Science and Medicine.

Duchenne muscular dystrophy is caused by a mutation to one of the longest genes in the body. When there is a DNA error in the dystrophin gene, the body doesn’t make the protein dystrophin, which serves as a sort of shock absorber for the muscle fiber. Since there are numerous places in the dystrophin gene where a mutation can occur, flexibility for gene-editing treatment is crucial.
Duchenne occurs in about 1 in every 5,000 boys, according to the Centers for Disease Control and Prevention. Duchenne muscular dystrophy is a progressive disease affecting both muscle used for movement and heart muscle, with patients typically succumbing before age 30 due to heart failure.
“CRISPR-Cpf1 gene-editing can be applied to a vast number of mutations in the dystrophin gene. Our goal is to permanently correct the underlying genetic causes of this terrible disease, and this research brings us closer to realizing that end,” Dr. Olson said.
“CRISPR-Cpf1 differs from CRISPR-Cas9 in a number of key ways, including being easier to deliver to muscle cells, said Yu Zhang, a graduate student in Dr. Olson’s lab and the first author of this study.
Other UT Southwestern researchers who contributed to this work are Dr. Hui Li, research scientist; John R. McAnally, research scientist; Dr. Kedryn Baskin, postdoctoral researcher; and John M. Shelton, senior research scientist.
Note: Dr. Rhonda Bassel-Duby and Dr. Eric Olson are consultants for Exonics Therapeutics. Drs. Olson, Bassel-Duby, Zhang, and Long are listed on the patent entitled “Prevention of muscular dystrophy by CRISPR/Cpf1-mediated gene editing” (U.S. Patent 62/426,853, 28 November 2016).
Funding: This work was supported by grants from the National Institutes of Health (NIH), a Paul D. Wellstone Muscular Dystrophy Cooperative Research Centers grant, and a Robert A. Welch Foundation grant.
Source: UT Southwestern
Image Source: NeuroscienceNews.com images are credited to the researchers.
Original Research: Full open access research for “CRISPR-Cpf1 correction of muscular dystrophy mutations in human cardiomyocytes and mice” by Yu Zhang, Chengzu Long, Hui Li, John R. McAnally, Kedryn K. Baskin, John M. Shelton, Rhonda Bassel-Duby, and Eric N. Olson in Science Advances. Published online April 12 2017 doi:10.1126/sciadv.1602814
[cbtabs][cbtab title=”MLA”]UT Southwestern “CRISPR Corrects Duchenne Muscular Dystrophy.” NeuroscienceNews. NeuroscienceNews, 13 April 2017.
<https://neurosciencenews.com/crispr-duchenne-6402/>.[/cbtab][cbtab title=”APA”]UT Southwestern (2017, April 13). CRISPR Corrects Duchenne Muscular Dystrophy. NeuroscienceNew. Retrieved April 13, 2017 from https://neurosciencenews.com/crispr-duchenne-6402/[/cbtab][cbtab title=”Chicago”]UT Southwestern “CRISPR Corrects Duchenne Muscular Dystrophy.” https://neurosciencenews.com/crispr-duchenne-6402/ (accessed April 13, 2017).[/cbtab][/cbtabs]
Abstract
CRISPR-Cpf1 correction of muscular dystrophy mutations in human cardiomyocytes and mice
Duchenne muscular dystrophy (DMD), caused by mutations in the X-linked dystrophin gene (DMD), is characterized by fatal degeneration of striated muscles. Dilated cardiomyopathy is one of the most common lethal features of the disease. We deployed Cpf1, a unique class 2 CRISPR (clustered regularly interspaced short palindromic repeats) effector, to correct DMD mutations in patient-derived induced pluripotent stem cells (iPSCs) and mdx mice, an animal model of DMD. Cpf1-mediated genomic editing of human iPSCs, either by skipping of an out-of-frame DMD exon or by correcting a nonsense mutation, restored dystrophin expression after differentiation to cardiomyocytes and enhanced contractile function. Similarly, pathophysiological hallmarks of muscular dystrophy were corrected in mdx mice following Cpf1-mediated germline editing. These findings are the first to show the efficiency of Cpf1-mediated correction of genetic mutations in human cells and an animal disease model and represent a significant step toward therapeutic translation of gene editing for correction of DMD.
“CRISPR-Cpf1 correction of muscular dystrophy mutations in human cardiomyocytes and mice” by Yu Zhang, Chengzu Long, Hui Li, John R. McAnally, Kedryn K. Baskin, John M. Shelton, Rhonda Bassel-Duby, and Eric N. Olson in Science Advances. Published online April 12 2017 doi:10.1126/sciadv.1602814







