Summary: Researchers use CRISPR gene editing technology to rewire stem cells in order to fight inflammation caused by arthritis.
Source: WUSTL.
Goal is vaccine that targets inflammation in joints.
Using new gene-editing technology, researchers have rewired mouse stem cells to fight inflammation caused by arthritis and other chronic conditions. Such stem cells, known as SMART cells (Stem cells Modified for Autonomous Regenerative Therapy), develop into cartilage cells that produce a biologic anti-inflammatory drug that, ideally, will replace arthritic cartilage and simultaneously protect joints and other tissues from damage that occurs with chronic inflammation.
The cells were developed at Washington University School of Medicine in St. Louis and Shriners Hospitals for Children-St. Louis, in collaboration with investigators at Duke University and Cytex Therapeutics Inc., both in Durham, N.C. The researchers initially worked with skin cells taken from the tails of mice and converted those cells into stem cells. Then, using the gene-editing tool CRISPR in cells grown in culture, they removed a key gene in the inflammatory process and replaced it with a gene that releases a biologic drug that combats inflammation.
The research is available online April 27 in the journal Stem Cell Reports.
“Our goal is to package the rewired stem cells as a vaccine for arthritis, which would deliver an anti-inflammatory drug to an arthritic joint but only when it is needed,” said Farshid Guilak, PhD, the paper’s senior author and a professor of orthopedic surgery at Washington University School of Medicine. “To do this, we needed to create a ‘smart’ cell.”
Many current drugs used to treat arthritis — including Enbrel, Humira and Remicade — attack an inflammation-promoting molecule called tumor necrosis factor-alpha (TNF-alpha). But the problem with these drugs is that they are given systemically rather than targeted to joints. As a result, they interfere with the immune system throughout the body and can make patients susceptible to side effects such as infections.
“We want to use our gene-editing technology as a way to deliver targeted therapy in response to localized inflammation in a joint, as opposed to current drug therapies that can interfere with the inflammatory response through the entire body,” said Guilak, also a professor of developmental biology and of biomedical engineering and co-director of Washington University’s Center of Regenerative Medicine. “If this strategy proves to be successful, the engineered cells only would block inflammation when inflammatory signals are released, such as during an arthritic flare in that joint.”
As part of the study, Guilak and his colleagues grew mouse stem cells in a test tube and then used CRISPR technology to replace a critical mediator of inflammation with a TNF-alpha inhibitor.
“Exploiting tools from synthetic biology, we found we could re-code the program that stem cells use to orchestrate their response to inflammation,” said Jonathan Brunger, PhD, the paper’s first author and a postdoctoral fellow in cellular and molecular pharmacology at the University of California, San Francisco.
Over the course of a few days, the team directed the modified stem cells to grow into cartilage cells and produce cartilage tissue. Further experiments by the team showed that the engineered cartilage was protected from inflammation.
“We hijacked an inflammatory pathway to create cells that produced a protective drug,” Brunger said.
The researchers also encoded the stem/cartilage cells with genes that made the cells light up when responding to inflammation, so the scientists easily could determine when the cells were responding. Recently, Guilak’s team has begun testing the engineered stem cells in mouse models of rheumatoid arthritis and other inflammatory diseases.
If the work can be replicated in animals and then developed into a clinical therapy, the engineered cells or cartilage grown from stem cells would respond to inflammation by releasing a biologic drug — the TNF-alpha inhibitor — that would protect the synthetic cartilage cells that Guilak’s team created and the natural cartilage cells in specific joints.
“When these cells see TNF-alpha, they rapidly activate a therapy that reduces inflammation,” Guilak explained. “We believe this strategy also may work for other systems that depend on a feedback loop. In diabetes, for example, it’s possible we could make stem cells that would sense glucose and turn on insulin in response. We are using pluripotent stem cells, so we can make them into any cell type, and with CRISPR, we can remove or insert genes that have the potential to treat many types of disorders.”
With an eye toward further applications of this approach, Brunger added, “The ability to build living tissues from ‘smart’ stem cells that precisely respond to their environment opens up exciting possibilities for investigation in regenerative medicine.”
Funding: This work was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute on Aging of the National Institutes of Health (NIH), grant numbers AR061042, AR50245, AR46652, AR48182, AR067467, AR065956, AG15768, OD008586. Additional funding provided by the Nancy Taylor Foundation for Chronic Diseases; the Arthritis Foundation; the National Science Foundation (NSF), CAREER award number CBET-1151035; and the Collaborative Research Center of the AO Foundation, Davos, Switzerland.
Note: Authors Farshid Guilak, and Vincent Willard have a financial interest in Cytex Therapeutics of Durham, N.C., which may choose to license this technology. Cytex is a startup founded by some of the investigators. They could realize financial gain if the technology eventually is approved for clinical use.
Source: Jim Dryden – WUSTL
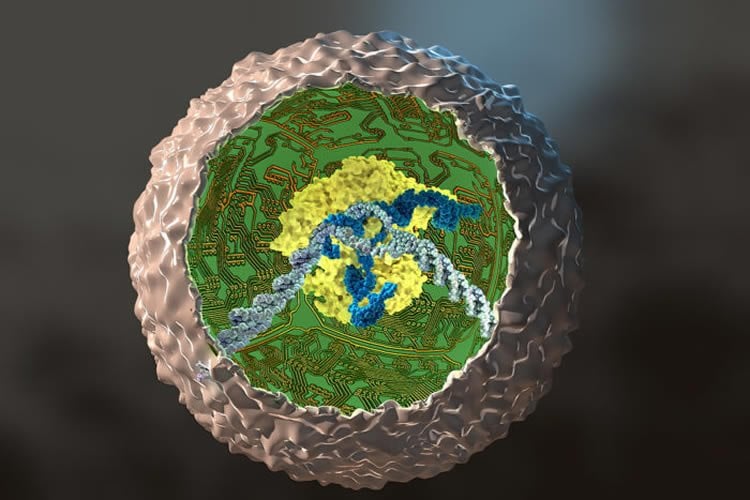
Image Source: NeuroscienceNews.com image is credited to Ella Marushchenko.
Original Research: Full open access research for “Genome Engineering of Stem Cells for Autonomously Regulated, Closed-Loop Delivery of Biologic Drugs” by Jonathan M. Brunger, Ananya Zutshi, Vincent P. Willard, Charles A. Gersbach, and Farshid Guilak in Stem Cell Reports. Published online April 27 2017 doi:10.1016/j.stemcr.2017.03.022
[cbtabs][cbtab title=”MLA”]WUSTL “CRISPR Used to Edit Stem Cells in Fight Against Arthritis: Brain Views Immoral Acts As If They Are Impossible.” NeuroscienceNews. NeuroscienceNews, 29 April 2017.
<https://neurosciencenews.com/crispr-arthritis-stem-cells-6543/>.[/cbtab][cbtab title=”APA”]WUSTL (2017, April 29). CRISPR Used to Edit Stem Cells in Fight Against Arthritis: Brain Views Immoral Acts As If They Are Impossible. NeuroscienceNew. Retrieved April 29, 2017 from https://neurosciencenews.com/crispr-arthritis-stem-cells-6543/[/cbtab][cbtab title=”Chicago”]WUSTL “CRISPR Used to Edit Stem Cells in Fight Against Arthritis: Brain Views Immoral Acts As If They Are Impossible.” https://neurosciencenews.com/crispr-arthritis-stem-cells-6543/ (accessed April 29, 2017).[/cbtab][/cbtabs]
Abstract
Genome Engineering of Stem Cells for Autonomously Regulated, Closed-Loop Delivery of Biologic Drugs
Highlights
•Stem cells were rewired via genome engineering to combat inflammation
•Cells were used to engineer tissues that self-regulate biologic drug production
•Autoregulated therapy protected tissues from cytokines that drive chronic diseases
•This approach can form the basis of a cellular vaccine for inflammatory diseases
Summary
Chronic inflammatory diseases such as arthritis are characterized by dysregulated responses to pro-inflammatory cytokines such as interleukin-1 (IL-1) and tumor necrosis factor α (TNF-α). Pharmacologic anti-cytokine therapies are often effective at diminishing this inflammatory response but have significant side effects and are used at high, constant doses that do not reflect the dynamic nature of disease activity. Using the CRISPR/Cas9 genome-engineering system, we created stem cells that antagonize IL-1- or TNF-α-mediated inflammation in an autoregulated, feedback-controlled manner. Our results show that genome engineering can be used successfully to rewire endogenous cell circuits to allow for prescribed input/output relationships between inflammatory mediators and their antagonists, providing a foundation for cell-based drug delivery or cell-based vaccines via a rapidly responsive, autoregulated system. The customization of intrinsic cellular signaling pathways in stem cells, as demonstrated here, opens innovative possibilities for safer and more effective therapeutic approaches for a wide variety of diseases.
“Genome Engineering of Stem Cells for Autonomously Regulated, Closed-Loop Delivery of Biologic Drugs” by Jonathan M. Brunger, Ananya Zutshi, Vincent P. Willard, Charles A. Gersbach, and Farshid Guilak in Stem Cell Reports. Published online April 27 2017 doi:10.1016/j.stemcr.2017.03.022






