Summary: Researchers report an exaggerated immune response can trigger chronic fatigue syndrome. The study reveals levels of Il-10 were higher in those who developed lasting fatigue, suggesting the immune system may have been primed to over respond.
Source: King’s College London.
New research from King’s College London finds that an exaggerated immune response can trigger long-lasting fatigue, potentially explaining how chronic fatigue syndrome (CFS) begins. The study is the most in-depth biological investigation yet into the role of the immune system in lasting symptoms of fatigue.
CFS, also known as myalgic encephalomyelitis (ME), is a long-term illness which is characterised by extreme tiredness. The underlying biology of CFS has remained a mystery, hampering the search for treatments. There is some evidence that the immune system plays a role in triggering CFS and many patients report their illness starting with a challenge to the immune system such as a viral illness.
By the time patients are diagnosed it is too late to catch CFS in its earliest stages, and it is impossible to assess the biology of patients before the illness develops. To get around this problem, researchers from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) used a model for CFS based on a treatment for hepatitis C called interferon-alpha.
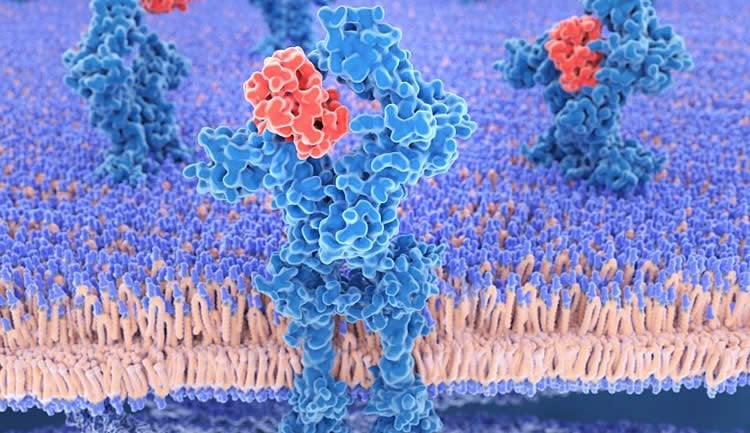
Interferon-alpha activates the immune system in the same way as a powerful infection. A lot of patients develop acute fatigue during treatment with interferon-alpha and a minority go on to have a CFS-like illness, where fatigue lasts for more than six months after the treatment ends. The researchers measured fatigue and immune system markers in 55 patients before, during and after treatment with interferon-alpha, tracking which people developed the persistent CFS-like illness.
The team found differences in the immune systems of 18 patients who developed lasting fatigue compared to those who recovered as normal. During treatment with interferon-alpha there was a much bigger immune response among those who developed the CFS-like illness, with a doubling in the levels of immune system ‘messenger’ molecules interleukin-10 and interleukin-6.
Importantly, even before treatment started, levels of interleukin-10 were higher among those who went on to have lasting fatigue, suggesting the immune system may have been ‘primed’ to over-respond.
Lead researcher Dr Alice Russell from the IoPPN says: ‘For the first time, we have shown that people who are prone to develop a CFS-like illness have an overactive immune system, both before and during a challenge to the immune system. Our findings suggest that people who have an exaggerated immune response to a trigger may be more at risk of developing CFS.’
By the time the CFS-like illness developed, however, there was no longer any detectable difference in the immune system of patients compared to those who recovered as normal. As well as looking at people having interferon-alpha treatment, the researchers also found no difference in immune activation between 54 people with diagnosed CFS and 57 healthy controls.
Alongside the overactive immune response, those people who developed the CFS-like illness had more acute fatigue during treatment with interferon-alpha than people who recovered as normal. Yet before treatment there was no difference between the groups in their levels of fatigue or in any psychiatric symptoms like depression or recent stressful life-events.
Senior researcher Professor Carmine Pariante from the IoPPN says: ‘A better understanding of the biology underlying the development of CFS is needed to help patients suffering with this debilitating condition. Although screening tests are a long way off, our results are the first step in identifying those at risk and catching the illness in its crucial early stages.’
Confirmation is needed that the findings from people treated with interferon-alpha apply to people with CFS, and future work to better understand the factors that may be driving an exaggerated immune response is required.
Dr Neha Issar-Brown, Head of Population and Systems Medicine at the Medical Research Council, which funded the research, said: ‘CFS/ME is a serious condition and its underpinning biology is poorly understood. Encouragingly, this work sheds light on potential mechanisms of immune dysregulation underlying early stages of chronic fatigue syndrome. The MRC strongly encourages more research to better understand this condition in order to address an area of unmet clinical need.’
Source: King’s College London
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is adapted from the King’s College London news release.
Original Research: Open access research for “Persistent fatigue induced by interferon-alpha: a novel, inflammation-based, proxy model of chronic fatigue syndrome” by Alice Russell, Nilay Hepgul, Naghmeh Nikkheslat, Alessandra Borsini, Zuzanna Zajkowska, Natalie Moll, Daniel Forton, Kosh Agarwal, Trudie Chaldera, Valeria Mondelli, Matthew Hotopf, Anthony Cleare, Gabrielle Murphy, Graham Foster, Terry Wong, Gregor A. Schütze, Markus J. Schwarz, Neil Harrison, Patricia A. Zunszain, and Carmine M. Pariantea in Psychoneuroendocrinology. Published December 17 2018.
doi:10.1016/j.psyneuen.2018.11.032
[cbtabs][cbtab title=”MLA”]King’s College London”Immune Response May Trigger Chronic Fatigue Syndrome.” NeuroscienceNews. NeuroscienceNews, 18 December 2018.
<https://neurosciencenews.com/chronic-fatigue-immune-10371/>.[/cbtab][cbtab title=”APA”]King’s College London(2018, December 18). Immune Response May Trigger Chronic Fatigue Syndrome. NeuroscienceNews. Retrieved December 18, 2018 from https://neurosciencenews.com/chronic-fatigue-immune-10371/[/cbtab][cbtab title=”Chicago”]King’s College London”Immune Response May Trigger Chronic Fatigue Syndrome.” https://neurosciencenews.com/chronic-fatigue-immune-10371/ (accessed December 18, 2018).[/cbtab][/cbtabs]
Abstract
Persistent fatigue induced by interferon-alpha: a novel, inflammation-based, proxy model of chronic fatigue syndrome
The role of immune or infective triggers in the pathogenesis of Chronic Fatigue Syndrome (CFS) is not yet fully understood. Barriers to obtaining immune measures at baseline (i.e., before the trigger) in CFS and post-infective fatigue model cohorts have prevented the study of pre-existing immune dysfunction and subsequent immune changes in response to the trigger.
This study presents interferon-alpha (IFN-α)-induced persistent fatigue as a model of CFS. IFN-α, which is used in the treatment of chronic Hepatitis C Virus (HCV) infection, induces a persistent fatigue in some individuals, which does not abate post-treatment, that is, once there is no longer immune activation. This model allows for the assessment of patients before and during exposure to the immune trigger, and afterwards when the original trigger is no longer present.
Fifty-five patients undergoing IFN-α treatment for chronic HCV were assessed at baseline, during the 6–12 months of IFN-α treatment, and at six-months post-treatment. Measures of fatigue, cytokines and kynurenine pathway metabolites were obtained. Fifty-four CFS patients and 57 healthy volunteers completed the same measures at a one-off assessment, which were compared with post-treatment follow-up measures from the HCV patients.
Eighteen patients undergoing IFN-α treatment (33%) were subsequently defined as having ‘persistent fatigue’ (the proposed model for CFS), if their levels of fatigue were higher six-months post-treatment than at baseline; the other 67% were considered ‘resolved fatigue’. Patients who went on to develop persistent fatigue experienced a greater increase in fatigue symptoms over the first four weeks of IFN-α, compared with patients who did not (Δ Treatment Week (TW)-0 vs. TW4; PF: 7.1 ± 1.5 vs. RF: 4.0 ± 0.8, p = 0.046). Moreover, there was a trend towards increased baseline interleukin (IL)-6, and significantly higher baseline IL-10 levels, as well as higher levels of these cytokines in response to IFN-α treatment, alongside concurrent increases in fatigue. Levels increased to more than double those of the other patients by Treatment Week (TW)4 (p = 0.011 for IL-6 and p = 0.001 for IL-10). There was no evidence of an association between persistent fatigue and peripheral inflammation six-months post-treatment, nor did we observe peripheral inflammation in the CFS cohort. While there were changes in kynurenine metabolites in response to IFN-α, there was no association with persistent fatigue. CFS patients had lower levels of the ratio of kynurenine to tryptophan and 3-hydroxykynurenine than controls.
Future studies are needed to elucidate the mechanisms behind the initial exaggerated response of the immune system in those who go on to experience persistent fatigue even if the immune trigger is no longer present, and the change from acute to chronic fatigue in the absence of continued peripheral immune activation.