Summary: Bartonella infection may contribute to progressive psychiatric symptoms associated with schizophrenia and PANS in a subset of patients.
Source: North Carolina State University
In a new case study, researchers at North Carolina State University describe an adolescent human patient diagnosed with rapid onset schizophrenia who was found instead to have a Bartonella henselae infection. This study adds to the growing body of evidence that Bartonella infection can mimic a host of chronic illnesses, including mental illness, and could open up new avenues of research into bacterial or microbial causes of mental disorders.
Bartonella is a bacteria most commonly associated with cat scratch disease, which until recently was thought to be a short-lived (or self-limiting) infection. There are at least 30 different known species of Bartonella, and 13 of those have been found to infect human beings. The ability to find and diagnose Bartonella infection in animals and humans – it is notorious for “hiding” in the linings of blood vessels – has led to its identification in patients with a host of chronic illnesses ranging from migraines to seizures to rheumatoid illnesses that the medical community previously hadn’t been able to attribute to a specific cause.
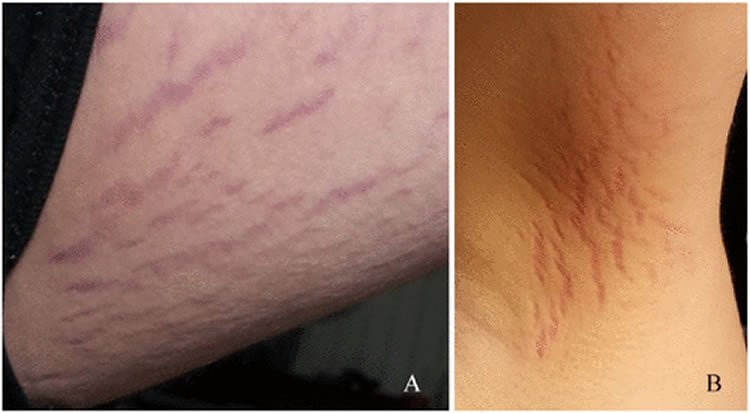
In a case study published in the Journal of Central Nervous System Disease, an adolescent with sudden onset psychotic behavior – diagnosed as schizophrenia – was seen and treated by numerous specialists and therapists over an 18-month period. All conventional treatments for both psychosis and autoimmune disorders failed. Finally, a physician recognized lesions on the patient’s skin that are often associated with Bartonella, and the patient tested positive for the infection. Combination antimicrobial chemotherapy led to full recovery.
“This case is interesting for a number of reasons,” says Dr. Ed Breitschwerdt, Melanie S. Steele Distinguished Professor of Internal Medicine at NC State and lead author of the case report. “Beyond suggesting that Bartonella infection itself could contribute to progressive neuropsychiatric disorders like schizophrenia, it raises the question of how often infection may be involved with psychiatric disorders generally.
“Researchers are starting to look at things like infection’s role in Alzheimer’s disease, for example. Beyond this one case, there’s a lot of movement in trying to understand the potential role of viral and bacterial infections in these medically complex diseases. This case gives us proof that there can be a connection, and offers an opportunity for future investigations.”
Co-authors of the study include NC State research associate professor Ricardo Maggi and research technician Julie Bradley, psychiatrist Dr. Rosalie Greenberg, rheumatologist Dr. Robert Mozayeni, and pediatrician Dr. Allen Lewis.
Funding: Funding was provided by the College of Veterinary Medicine Bartonella/Vector Borne Disease Research Fund.
Source:
North Carolina State University
Media Contacts:
Tracey Peake – North Carolina State University
Image Source:
The image is credited to Breitschwerdt et al./Journal of Central Nervous System Disease.
Original Research: Open access
Breitschwerdt, E. B., Greenberg, R., Maggi, R. G., Mozayeni, B. R., Lewis, A., & Bradley, J. M. (2019). “Bartonella henselae Bloodstream Infection in a Boy With Pediatric Acute-Onset Neuropsychiatric Syndrome”. Journal of Central Nervous System Disease. doi:10.1177/1179573519832014
Abstract
Bartonella henselae Bloodstream Infection in a Boy With Pediatric Acute-Onset Neuropsychiatric Syndrome
Background:
With the advent of more sensitive culture and molecular diagnostic testing modalities, Bartonella spp. infections have been documented in blood and/or cerebrospinal fluid specimens from patients with diverse neurological symptoms. Pediatric acute-onset neuropsychiatric syndrome (PANS) is characterized by an unusually abrupt onset of cognitive, behavioral, or neurological symptoms. Between October 2015 and January 2017, a 14-year-old boy underwent evaluation by multiple specialists for sudden-onset psychotic behavior (hallucinations, delusions, suicidal and homicidal ideation).
Methods:
In March 2017, Bartonella spp. serology (indirect fluorescent antibody assays) and polymerase chain reaction (PCR) amplification, DNA sequencing, and Bartonella enrichment blood culture were used on a research basis to assess Bartonella spp. exposure and bloodstream infection, respectively. PCR assays targeting other vector-borne infections were performed to assess potential co-infections.
Results:
For 18 months, the boy remained psychotic despite 4 hospitalizations, therapeutic trials involving multiple psychiatric medication combinations, and immunosuppressive treatment for autoimmune encephalitis. Neurobartonellosis was diagnosed after cutaneous lesions developed. Subsequently, despite nearly 2 consecutive months of doxycycline administration, Bartonella henselae DNA was PCR amplified and sequenced from the patient’s blood, and from Bartonella alphaproteobacteria growth medium enrichment blood cultures. B henselae serology was negative. During treatment with combination antimicrobial chemotherapy, he experienced a gradual progressive decrease in neuropsychiatric symptoms, cessation of psychiatric drugs, resolution of Bartonella-associated cutaneous lesions, and a return to all pre-illness activities.
Conclusions:
This case report suggests that B henselae bloodstream infection may contribute to progressive, recalcitrant neuropsychiatric symptoms consistent with PANS in a subset of patients.