Summary: Researchers have discovered that people with Alzheimer’s show unusually high neural flexibility—the constant reorganizing of brain networks—even while resting. In a large study of older adults, higher neural flexibility in the visual network predicted which healthy participants would later develop dementia.
This finding suggests that measuring brain reorganization may serve as an early biomarker for Alzheimer’s risk. While still experimental, the results also highlight the brain’s adaptability, even in the face of disease.
Key Facts
- Neural Flexibility: Alzheimer’s patients reorganize brain networks more often than healthy individuals.
- Predictive Power: High flexibility in visual networks predicted transition to Alzheimer’s years later.
- Hope & Resilience: Despite disease progression, the brain shows dynamic adaptability.
Source: University of Michigan
Some regions of the brain in people with Alzheimer’s reorganize more often while at rest than in people without the disease––and in healthy people this frequent reshuffling sometimes predicts who will develop the condition later, according to a new study from the University of Michigan and Columbia University.
The brain’s ability to reorganize various regions is called neural flexibility, says Eleanna Varangis, assistant professor at the U-M School of Kinesiology and first author of the study, which appears in the Journal of Alzheimer’s Disease.
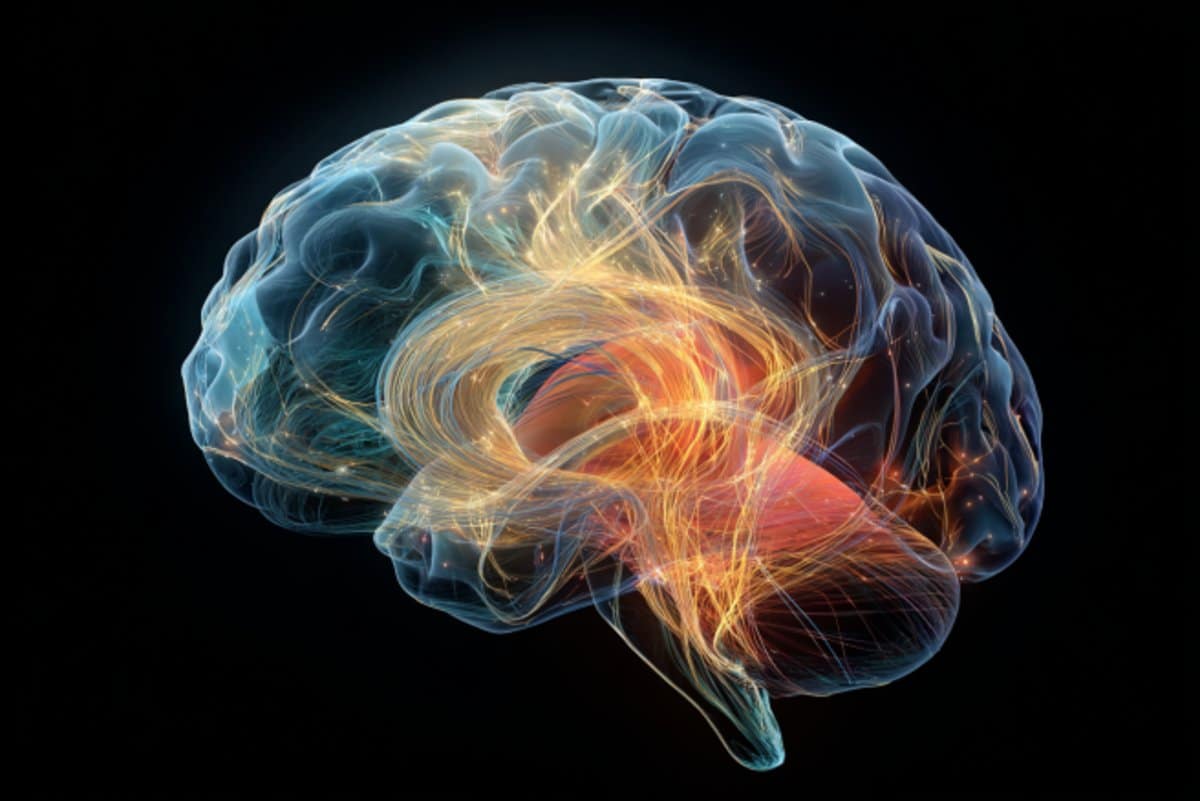
“Our brain is always organizing and reorganizing regions into different functional networks in order to make sure it has the resources it needs to complete a variety of cognitive tasks,” said Varangis, who is also a member of the Michigan Concussion Center.
“We found that in Alzheimer’s disease the brain tends to reorganize more frequently.
“Overall, our paper suggests that we can use information about the way our brain organizes into functional networks to possibly help identify whether or not someone has Alzheimer’s disease.”
It’s thought that 1 in 10 men and 1 in 5 women will develop Alzheimer’s disease in their lifetime, and early intervention is critical to maintain independence. Functional brain imaging has shown potential as an early biomarker of disease risk, Varangis says.
In this study, which was supported by the National Institutes of Health and the Brain & Behavior Research Foundation, researchers used functional MRI data collected while participants were awake but resting to examine neural flexibility in the brains of 862 older adults in the Alzheimer’s Disease Neuroimaging Initiative, across three groups: cognitively normal; mild cognitive impairment; and those with Alzheimer’s disease.
Varangis and colleagues wanted to know two things: if the damage to the brain caused by Alzheimer’s disease caused changes in neural flexibility; and if neural flexibility could be used to help predict who from the cognitively normal group would transition to Alzheimer’s disease.
They found that neural flexibility was significantly higher in the Alzheimer’s group than in the cognitively normal group across all brain regions and in six specific networks, and neural flexibility was significantly higher in the mild cognitive impairment group than in the cognitively normal group in the visual network.
Among the 617 healthy participants at baseline, 8.6% converted to dementia over the next 11 years, in keeping with national estimates of dementia prevalence in older age. Higher neural flexibility in the visual network was associated with transition to Alzheimer’s disease.
“While this was only a modest effect, it is a good hint that activity in these visual regions may be telling us something about risk for Alzheimer’s disease years before formal diagnosis,” Varangis said.
“Since we think of cognitive impairment being the primary symptom of Alzheimer’s disease, the finding that this sensory network was the one that predicted Alzheimer’s conversion was a bit unexpected, but it wasn’t necessarily surprising.
“In typical Alzheimer’s disease, the brain pathology that causes the disease does not progress to sensory regions until later stages of the disease. It could be that these regions show more flexibility because they are among the healthier regions of the brain that have not yet been affected by Alzheimer’s disease pathology.”
The findings challenged the researchers’ intuition because generally speaking, flexibility and adaptability are thought of as good things, Varangis says.
“But once we see the disease process setting in, it could be the case that if we’re just resting and we are showing this frequent reassignment of brain regions to different functions it could be that parts of the brain aren’t working the way that they should be,” she said.
It’s important to remember that this is an experimental technique and is far from being a diagnostic application, Varangis says.
“The positive here is that I think a lot of people think that in neurodegenerative disease you see this general brain slowing over time,” she said.
“But to me, these findings also speak to the fact that the brain is such a dynamic organ, that even when folks are experiencing these cognitive changes or getting worse over time, there’s so much flexibility for our brains to adapt, which I think is also a sign of hope and resilience.”
Co-authors include: Jun Liu, Yuqi Miao, Xi Zhu, Yaakov Stern, Seonjoo Lee, all associated with Columbia University.
Funding: The work was funded by grants from the National Institutes of Health [R01AG062578 (PI: Lee), NIH K01MH122774] and a Brain & Behavior Research Foundation NARSAD Young Investigator Grant (PI: Zhu).
About this Alzheimer’s disease research news
Author: Laura Bailey
Source: University of Michigan
Contact: Laura Bailey – University of Michigan
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Neural flexibility is higher in Alzheimer’s disease and predicts Alzheimer’s disease transition” by Eleanna Varangis et al. Journal of Alzheimer’s Disease
Abstract
Neural flexibility is higher in Alzheimer’s disease and predicts Alzheimer’s disease transition
Background
Neural flexibility (NF), a measure of dynamic functional connectivity, was associated with psychiatric diseases but has not yet been studied in Alzheimer’s disease (AD).
Objective
We aim to evaluate whether AD is associated with alterations in NF and probe its predictive utility for AD conversion.
Method
The study included 862 older adults (461 cognitively normal (CN), 294 mild cognitive impairment (MCI), 107 AD) with valid resting-state fMRI data from the Alzheimer’s Disease Neuroimaging Initiative. We defined the NF of a node as the number of times that a node changed its community assignment across the sliding windows, normalized by the total number of possible changes.
We computed global NF and 12 functional network-specific NFs, then performed linear mixed models on NFs separately to explore the differences in these measures between our three groups. Finally, we evaluated the predictive utility of NF on dementia transition using survival analysis.
Results
NF is significantly higher in AD than CN on global NF (β = 0.002, 95% CI 0.001 to 0.004), and NF in six networks, and NF is significantly higher in MCI than CN in the visual network. Among n = 617 non-demented participants at baseline, n = 53 (8.6%) participants converted to dementia during the follow-up visits. Higher NF in the visual network was positively associated with AD transition (HR = 1.323, 95%CI 1.002 to 1.747, p = 0.049, per 1 SD in NF), controlling for age, gender, and education.
Conclusions
We found that NF during rest was higher in AD patients and predicted dementia transition. Thus, NF may be a valuable biomarker of AD; however, more validation and mechanistic studies need to be performed.