Summary: Researchers have advanced our understanding of how traumatic brain injuries (TBI) contribute to neurodegenerative diseases using lab-grown brain organoids. By simulating TBI in organoids derived from human stem cells, the team observed nerve cell death and pathological changes similar to those in TBI patients, particularly in proteins associated with ALS and dementia.
The discovery of the gene KCNJ2 as a protective factor against TBI effects opens new avenues for treatments. This study, supported by a blend of federal and private funding, underscores the potential of organoids in medical research and the critical role of genetics in TBI outcomes.
Key Facts:
- Simulated TBIs in brain organoids show pathological changes mirroring those in patients, highlighting a genetic predisposition to neurodegenerative diseases post-injury.
- The gene KCNJ2, involved in potassium ion transport, was identified as a protective agent against TBI-induced nerve cell death in both organoids and mouse models.
- The research, combining federal and private funding, demonstrates the value of brain organoids in exploring the mechanisms of TBI and identifying potential therapeutic targets.
Source: USC
A traumatic brain injury (TBI) can quadruple your risk for developing dementia and increase your chances of developing neurodegenerative diseases such as ALS.
In a new study published in Cell Stem Cell, USC scientists use lab-grown human brain structures known as organoids to offer insights into why this is the case and how to mitigate the risk.
In the study, former postdoc Jesse Lai and PhD student Joshua Berlind from the USC Stem Cell laboratory of Justin Ichida used human patient-derived stem cells to grow rudimentary brain structures known as organoids in the lab. They then injured these organoids with high-intensity ultrasound waves.

The injured organoids showed some of the same features seen in TBI patients, including nerve cell death and pathological changes in tau proteins, as well as in a protein called TDP-43.
The scientists found that the pathological changes in TDP-43 were more prevalent in organoids derived from patients with ALS or frontotemporal dementia, making their nerve cells more suspectable to dysfunction and death following injury.
This suggests that TBI might increase the risk of developing these diseases even more for patients with a genetic predisposition. The worst injuries were sustained by nerve cells that share information—called excitatory neurons—located in the deep layers of the organoids.
In their search for ways to protect these neurons against the effects of TBI, the scientists identified a gene called KCNJ2, which contains instructions for making channels that selectively allow potassium to pass through the cell membrane, helping to enable muscle contraction and relaxation.
Inhibiting this gene had a protective effect on organoids derived from patients with and without ALS, as well as on mice, following a TBI.
“Targeting KCNJ2 may reduce the death of nerve cells after TBI,” said Ichida, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at USC, and a principal investigator at the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC.
“This could have potential as either a post-injury treatment or as a prophylactic for athletes and others at high risk for TBI.”
About the authors and the study
Co-corresponding author Ichida is also a co-founder of AcuraStem and Modulo Bio, a Scientific Advisory Board (SAB) member at Spinogenix and Vesalius Therapeutics, and an employee in the Research and Early Development group at BioMarin Pharmaceutical. Co-corresponding author Lai and co-author Violeta Yu were both employees of Amgen during the study, and currently work at Dewpoint Therapeutics. Named companies were not involved in this research project.
First author Berlind is a PhD student in the Ichida Lab. Additional co-authors are Gabriella Fricklas, Cecilia Lie, Jean-Paul Urenda, Kelsey Lam, Naomi Sta Maria, Russell Jacobs, and Zhen Zhao from USC.
Funding: Fifty percent of the work was supported by federal funding from the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (grant F31NS117075), NINDS (grant R01 1R01NS097850-01), and the Department of Defense (grant 12907280). The project was also privately funded by an Amgen postdoctoral fellowship, the New York Stem Cell Foundation, the Tau Consortium, the Harrington Discovery Institute, the Alzheimer’s Drug Discovery Foundation, the Association for Frontotemporal Dementia, and the John Douglas French Alzheimer’s Foundation.
About this neurology and genetics research news
Author: Laura LeBlanc
Source: USC
Contact: Laura LeBlanc – USC
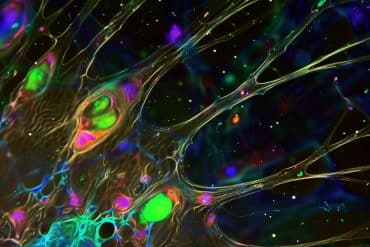
Image: The image is credited to Neuroscience News
Original Research: Open access.
“KCNJ2 inhibition mitigates mechanical injury in human brain organoids” by Jesse Lai et al. Cell Stem Cell
Abstract
KCNJ2 inhibition mitigates mechanical injury in human brain organoids
Highlights
- Mechanically injured organoids display hallmark features of traumatic brain injury
- TDP-43 dysfunction is a key driver of acute injury and is enhanced in ALS/FTD
- A CRISPRi screen identifies KCNJ2 inhibition as a therapeutic target in vitro
- Kcnj2 knockdown in mice reduces TDP-43 pathology and is protective against brain injury
Summary
Traumatic brain injury (TBI) strongly correlates with neurodegenerative disease. However, it remains unclear which neurodegenerative mechanisms are intrinsic to the brain and which strategies most potently mitigate these processes.
We developed a high-intensity ultrasound platform to inflict mechanical injury to induced pluripotent stem cell (iPSC)-derived cortical organoids. Mechanically injured organoids elicit classic hallmarks of TBI, including neuronal death, tau phosphorylation, and TDP-43 nuclear egress.
We found that deep-layer neurons were particularly vulnerable to injury and that TDP-43 proteinopathy promotes cell death. Injured organoids derived from C9ORF72 amyotrophic lateral sclerosis/frontotemporal dementia (ALS/FTD) patients displayed exacerbated TDP-43 dysfunction.
Using genome-wide CRISPR interference screening, we identified a mechanosensory channel, KCNJ2, whose inhibition potently mitigated neurodegenerative processes in vitro and in vivo, including in C9ORF72 ALS/FTD organoids.
Thus, targeting KCNJ2 may reduce acute neuronal death after brain injury, and we present a scalable, genetically flexible cerebral organoid model that may enable the identification of additional modifiers of mechanical stress.