Summary: A new study looks at the epigenetic factors that contribute to drug addiction and influence relapse.
Source: Medical University of South Carolina.
Why do some drug users continue to seek out drugs despite the prospect of losing family, friends, health or livelihood?
There are notable features — cues — of the early drug-using environment that often develop into persistent and powerful triggers for relapse. Epigenetic factors — enzymes in the brain that alter the packaging and accessibility of genes without changing the genes themselves — influence this process, according to research at the Medical University of South Carolina (MUSC) appearing online on September 27, 2017 in Neuron.
A major challenge in addiction science is to understand how transient experiences lead to long-lasting risk for relapse in users who try to quit, according to MUSC professor Christopher W. Cowan, Ph.D., William E. Murray SmartState® Endowed Chair in Neuroscience, and senior researcher on the project. “Our goal was to discover the brain mechanisms responsible for the rewarding effects of the drug and the motivation to seek it even after long periods of abstinence,” says Cowan.
The brains of drug users who have progressed to addiction differ markedly from those of early or casual users. Long-lasting associations form between the early use of a drug and different aspects of the early drug-using environment, such as the location in which a drug was first taken or the emotions a user was experiencing at the time. This can cause addicted users who have quit to experience cravings when in a similar setting. Understanding these connections could lead to better treatments for addiction.
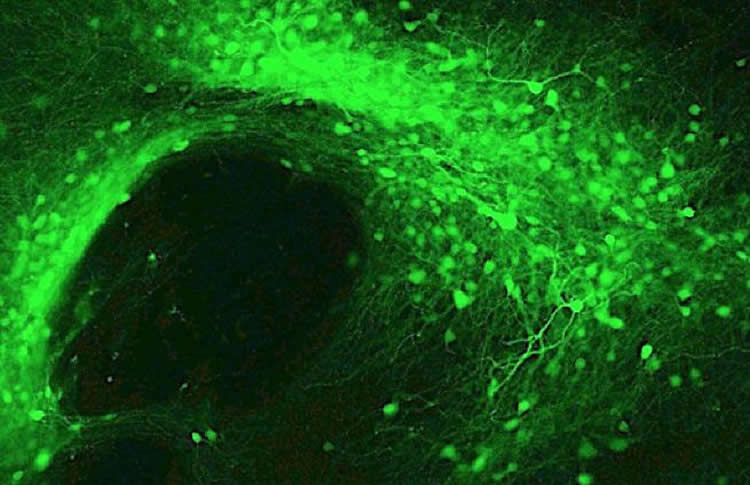
Cowan’s challenge was to determine which genes were activated in the early drug-using environment. Cowan and his fellow researchers had previously found that the epigenetic enzyme histone deacetylase 5 (HDAC5) slows the rodent brain from forming associations between cocaine and simple cues in the environment, such as light and sound. HDAC5 is found in high amounts in neurons in the nucleus accumbens, part of the reward center of the brain that reacts strongly to cocaine, opioids and alcohol — both in rodents and humans. When HDACs are in the nucleus of neurons, they change the way genomic DNA is packaged in the cell nucleus and often block the ability of certain genes to be turned on.
In the new study, rodents were trained to press a lever to receive a dose of cocaine. Each time they received a dose, a lamp went on above the lever and a brief sound was generated. These served as simple environmental cues for drug use. Next, some rodents were given a form of HDAC5 that traveled straight to the nuclei of neurons. Those rodents still pressed the lever just as many times to receive drug, meaning that HDAC5, on its own, was likely not blocking genes that promoted early drug-seeking behavior.
Yet the next experiment proved that HDAC5 reduced drug-seeking behavior during abstinence. To simulate withdrawal and abstinence, rodents were given rest without cocaine for one week, followed by a period during which they had access to the lever again. To simulate relapse, the rodents were shown the environmental cues again, this time without having pressed the lever. The presentation of the cues triggered robust lever pressing, indicating drug seeking, in control animals, proving that the associations between drug and environment persisted in their brains. In contrast, animals who had the nuclear form of HDAC5 did not press the lever nearly as often, even after the experimenters gave the animals a small priming dose of cocaine, which often produces strong drug-seeking behaviors.
HDAC5, the gene suppressor, did not prevent addiction-like behaviors from forming, but it did prevent later drug seeking and relapse during abstinence — at least in rodents.
The researchers next used a cutting-edge technique that encourages epigenetic enzymes to bind to DNA, allowing them to identify all the genes inhibited by HDAC5. The gene for NPAS4 was a top hit, and significant for an important reason: it is an early-onset gene, meaning that its effects could be exerted on the brain rapidly unless HDAC5 was there to inhibit it — just the molecular event Cowan and his team were seeking.
In similar experiments, animals with less NPAS4 in the nucleus accumbens took more time to form those early connections between environmental cues and cocaine, but they still sought the drug just as often during later simulated relapse. Apparently, NPAS4 accounts for some addiction-related learning and memory processes in the brain, but not all of them, meaning that HDAC5 must be regulating additional genes that reduce relapse events. Cowan thinks uncovering additional downstream genes could help researchers untangle the details of how the brain transitions from early drug use to addiction, and how new treatments might be developed to reduce relapse in individuals suffering from substance use disorders.
Animals in the research setting may not mimic the full complexity of human addiction. However, abstinent patients report cravings when given reminders of their drug-associated environment or cues, and animals and humans share similar enzyme pathways and brain structures. Perhaps most exciting for addiction research is that these processes may be similar in the transition to cocaine, alcohol and opioid addictions. “We might have tapped into a mechanism with relevance to multiple substance use disorders,” says Cowan.
Funding: The study was funded by John Kaneb Fellowship, Fugaku Trust for Medicinal Research, Brain & Behavior Research Foundation, Eleanor and Miles Shore HMS Fellowship, Phyllis and Jerome Lyle Rappaport Foundation, FRAXA Foundation
Source: Heather Woolwine – Medical University of South Carolina
Image Source: NeuroscienceNews.com image is credited to Dr. Christopher Cowan, Medical University of South Carolina.
Original Research: The study will appear in Neuron.
[cbtabs][cbtab title=”MLA”]Medical University of South Carolina “Epigenetics of Addiction: Untangling Relapse and Addiction in the Brain.” NeuroscienceNews. NeuroscienceNews, 27 September 2017.
<https://neurosciencenews.com/epigenetics-relapse-addiction-7597/>.[/cbtab][cbtab title=”APA”]Medical University of South Carolina (2017, September 27). Epigenetics of Addiction: Untangling Relapse and Addiction in the Brain. NeuroscienceNews. Retrieved September 27, 2017 from https://neurosciencenews.com/epigenetics-relapse-addiction-7597/[/cbtab][cbtab title=”Chicago”]Medical University of South Carolina “Epigenetics of Addiction: Untangling Relapse and Addiction in the Brain.” https://neurosciencenews.com/epigenetics-relapse-addiction-7597/ (accessed September 27, 2017).[/cbtab][/cbtabs]