Summary: Less muscle mass and increased body fat may affect cognition as we age. The link between body mass and declining fluid intelligence may be attributed to different types of white blood cells.
Source: Iowa State University
Iowa State researchers have found for the first time that less muscle and more body fat may affect how flexible our thinking gets as we become older, and changes in parts of the immune system could be responsible.
These findings could lead to new treatments that help maintain mental flexibility in aging adults with obesity, sedentary lifestyles, or muscle loss that naturally happens with aging.
The study, led by Auriel Willette, assistant professor of food science and human nutrition, and Brandon Klinedinst, a PhD student in neuroscience, looked at data from more than 4,000 middle-aged to older UK Biobank participants, both men and women. The researchers examined direct measurements of lean muscle mass, abdominal fat, and subcutaneous fat, and how they were related to changes in fluid intelligence over six years.
Willette and Klinedinst discovered people mostly in their 40s and 50s who had higher amounts of fat in their mid-section had worse fluid intelligence as they got older. Greater muscle mass, by contrast, appeared to be a protective factor. These relationships stayed the same even after taking into account chronological age, level of education, and socioeconomic status.
“Chronological age doesn’t seem to be a factor in fluid intelligence decreasing over time,” Willette said. “It appears to be biological age, which here is the amount of fat and muscle.”
Generally, people begin to gain fat and lose lean muscle once they hit middle age, a trend that continues as they get older. To overcome this, implementing exercise routines to maintain lean muscle becomes more important. Klinedinst said exercising, especially resistance training, is essential for middle-aged women, who naturally tend to have less muscle mass than men.
The study also looked at whether or not changes in immune system activity could explain links between fat or muscle and fluid intelligence. Previous studies have shown that people with a higher body mass index (BMI) have more immune system activity in their blood, which activates the immune system in the brain and causes problems with cognition. BMI only takes into account total body mass, so it has not been clear whether fat, muscle, or both jump-start the immune system.
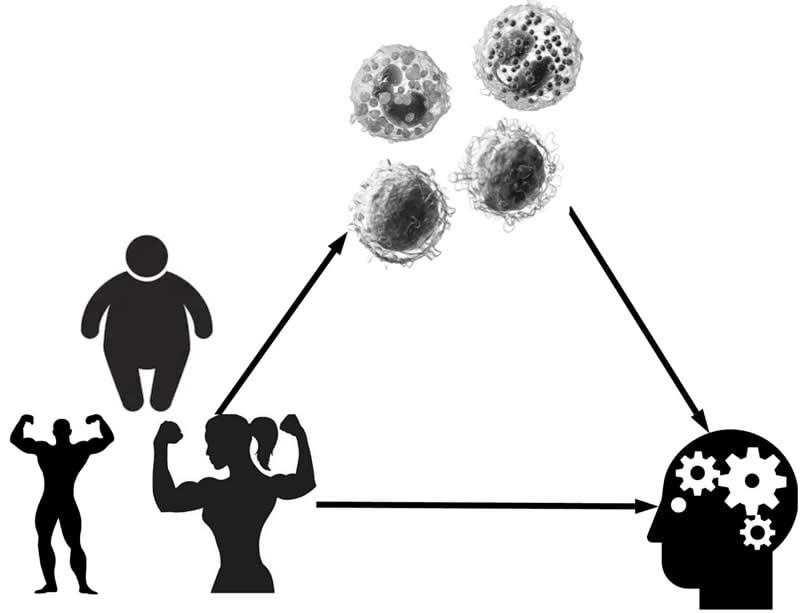
In this study, in women, the entire link between more abdominal fat and worse fluid intelligence was explained by changes in two types of white blood cells: lymphocytes and eosinophils. In men, a completely different type of white blood cell, basophils, explained roughly half of the fat and fluid intelligence link. While muscle mass was protective, the immune system did not seem to play a role.
While the study found correlations between body fat and decreased fluid intelligence, it is unknown at this time if it could increase the risk of Alzheimer’s disease.
“Further studies would be needed to see if people with less muscle mass and more fat mass are more likely to develop Alzheimer’s disease, and what the role of the immune system is,” Klinedinst said.
Starting a New Year’s resolution now to work out more and eat healthier may be a good idea, not only for your overall health, but to maintain healthy brain function.
“If you eat alright and do at least brisk walking some of the time, it might help you with mentally staying quick on your feet,” Willette said.
Source:
Iowa State University
Media Contacts:
Auriel Willette – Iowa State University
Image Source:
The image is credited to Auriel Willette, Iowa State University.
Original Research: Closed access
“Aging-related changes in fluid intelligence, muscle and adipose mass, and sex-specific immunologic mediation: A longitudinal UK Biobank study”. Auriel Willette et al.
Brain, Behavior, and Immunity doi:10.1016/j.bbi.2019.09.008.
Abstract
Aging-related changes in fluid intelligence, muscle and adipose mass, and sex-specific immunologic mediation: A longitudinal UK Biobank study
Background
Obesity in midlife and early late-life is associated with worse normal cognitive aging. Dual-energy X-ray absorptiometry (DEXA) suggests that visceral adipose mass (VAM) plays a predominant role, whereas non-visceral adipose mass (NVAM) and lean muscle mass (LMM) have shown conflicting relationships. It is unknown how longitudinal, cognitive changes in age-sensitive domains like fluid intelligence (FI) correspond to VAM, NVAM, and LMM in women and men. Furthermore, changes over time in blood leukocyte sub-populations may partially or fully account for sex-specific associations.
Methods
Data on 4431 late middle-aged, cognitively unimpaired adults (mean = 64.5 y) was obtained from the UK Biobank prospective cohort across 22 centers. FI scores, blood leukocyte counts, and covariates (age, social class, education) were measured at three 2-year intervals over 6 years. DEXA collection overlapped with these intervals. Sex-stratified growth curves, structural equations, and Preacher-Hayes mediation were used to estimate direct and indirect effects. β-weights were standardized.
Results
More LMM predicted gains in FI scores among women (β = 0.130, p < .001) and men (β = 0.089, p < .001). Conversely, more VAM and NVAM independently predicted FI decline equally among sexes (e.g., NVAM: women: β = −0.082, p < .001; men: β = −0.076, p < .001). Among women, FI associations were fully mediated by higher eosinophil counts via VAM (λ = 30.8%, p = .028) and lower lymphocyte counts via LMM (λ = 69.2%, p = .021). Among men, FI associations were partially mediated by lower basophils counts via LMM (λ = 4.5%, p = .042) and higher counts via VAM (λ = 50%, p = .037).
Conclusion
The proportion of LMM and VAM equally influenced male FI changes over 6 years, whereas higher LMM among women appeared to more strongly influence.
FI changes. Leukocyte counts strongly mediated VAM- and LMM-related FI changes in a sex-specific manner, but not for NVAM. For clinical translation, exercise studies in older adults may benefit from assessing sex-specific values of DEXA-based tissue mass, FI, and leukocyte sub-populations to gauge potential cognitive benefits of less VAM and more LMM.






