Summary: Researchers have identified a brain biomarker that may predict psychosis onset before symptoms appear, enabling earlier interventions and personalized care. MRI scans revealed abnormal connectivity patterns in sensory brain networks, with weaker connections between sensory regions and stronger connections to the thalamus.
This “somato-visual” biomarker was reliable across multiple scans and resilient to common confounds like medication or stress. The findings provide a foundation for timely psychosis diagnosis and could stratify patients into meaningful subgroups for targeted treatments.
Key Facts:
- A “somato-visual” biomarker identifies dysconnectivity in sensory brain networks.
- This biomarker was robust across scans and resistant to medication or stress effects.
- A five-minute MRI scan could enable earlier psychosis diagnosis and interventions.
Source: University of Rochester
The current standard of care for psychosis is a diagnostic interview, but what if it could be diagnosed before the first symptom emerged?
Researchers at the Del Monte Institute for Neuroscience at the University of Rochester are pointing toward a potential biomarker in the brain that could lead to more timely interventions and personalized care.

“Establishing such biomarkers could provide a key step in changing how we care for, treat, and offer interventions to people with psychosis,” said Brian Keane, PhD, assistant professor of Psychiatry, Center for Visual Science, and Neuroscience at the University of Rochester Medical Center. Keane recently co-authored an article in Molecular Psychiatry that identifies how MRI scans could reveal brain differences in people with psychosis.
“Aside from potentially predicting future psychosis onset, biomarkers could also help stratify patients into clinically meaningful subgroups and suggest new options for treatment or intervention.”
Using data collected by the Human Connectome Early Psychosis Project, researchers looked at MRI scans from 159 participants. These included 105 who developed a psychotic disorder up to five years prior to testing.
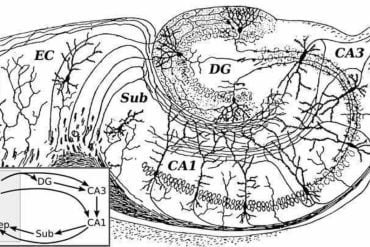
In the brains of participants with psychosis, researchers found that sensory regions in the cortex were more weakly connected to each other and more strongly connected to the thalamus, the brain’s information relay station.
These differences were confined to the somatomotor network, which processes bodily movement and sensations, and a visual network, which generates representations of objects, faces, and complex features. Combining the dysconnectivity patterns across these two networks allowed the researchers to create a “somato-visual” biomarker.
Previous research has suggested that abnormal brain connectivity exists prominently in the sensory networks of people with schizophrenia, but it remained unclear which networks were most responsible or whether dysconnectivity could be explained by other illness factors, such as antipsychotic use, anxiety, or stress.
“What makes this biomarker unique is its large effect size, its robustness to over a dozen common confounds, and its high reliability across multiple scans.
“A single five-minute scan could potentially improve our ability to predict which at-risk individuals will transition to a psychotic disorder, which in turn could allow for more timely treatments or interventions,” Keane said.
“It also gives us a place to keep looking. An important next step will be to determine if the somato-visual biomarker emerges before or as psychosis begins.”
Additional authors include Yonatan Abrham, Boyang Hu, and Brent Johnson of the University of Rochester, Carrisa Cocuzza of Yale University, and Michael Cole of Rutgers University. This work was supported by a K01 grant and a Psychiatry Department pilot grant at the University of Rochester.
About this psychosis and neuroscience research news
Author: Kelsie Smith Hayduk
Source: University of Rochester
Contact: Kelsie Smith Hayduk – University of Rochester
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Functional dysconnectivity of visual and somatomotor networks yields a simple and robust biomarker for psychosis” by Yonatan Abrham et al. Molecular Psychiatry
Abstract
Functional dysconnectivity of visual and somatomotor networks yields a simple and robust biomarker for psychosis
People with psychosis exhibit thalamo-cortical hyperconnectivity and cortico-cortical hypoconnectivity with sensory networks, however, it remains unclear if this applies to all sensory networks, whether it arises from other illness factors, or whether such differences could form the basis of a viable biomarker.
To address the foregoing, we harnessed data from the Human Connectome Early Psychosis Project and computed resting-state functional connectivity (RSFC) matrices for 54 healthy controls and 105 psychosis patients.
Primary visual, secondary visual (“visual2”), auditory, and somatomotor networks were defined via a recent brain network partition. RSFC was determined for 718 regions via regularized partial correlation.
Psychosis patients—both affective and non-affective—exhibited cortico-cortical hypoconnectivity and thalamo-cortical hyperconnectivity in somatomotor and visual2 networks but not in auditory or primary visual networks.
When we averaged and normalized the visual2 and somatomotor network connections, and subtracted the thalamo-cortical and cortico-cortical connectivity values, a robust psychosis biomarker emerged (p = 2e-10, Hedges’ g = 1.05).
This “somato-visual” biomarker was present in antipsychotic-naive patients and did not depend on confounds such as psychiatric comorbidities, substance/nicotine use, stress, anxiety, or demographics. It had moderate test-retest reliability (ICC = 0.62) and could be recovered in five-minute scans.
The marker could discriminate groups in leave-one-site-out cross-validation (AUC = 0.79) and improve group classification upon being added to a well-known neurocognition task. Finally, it could differentiate later-stage psychosis patients from healthy or ADHD controls in two independent data sets.
These results introduce a simple and robust RSFC biomarker that can distinguish psychosis patients from controls by the early illness stages.