Summary: According to researchers, Parkinson’s disease may start in the gut and spread to the brain via the vagus nerve.
Source: AAN.
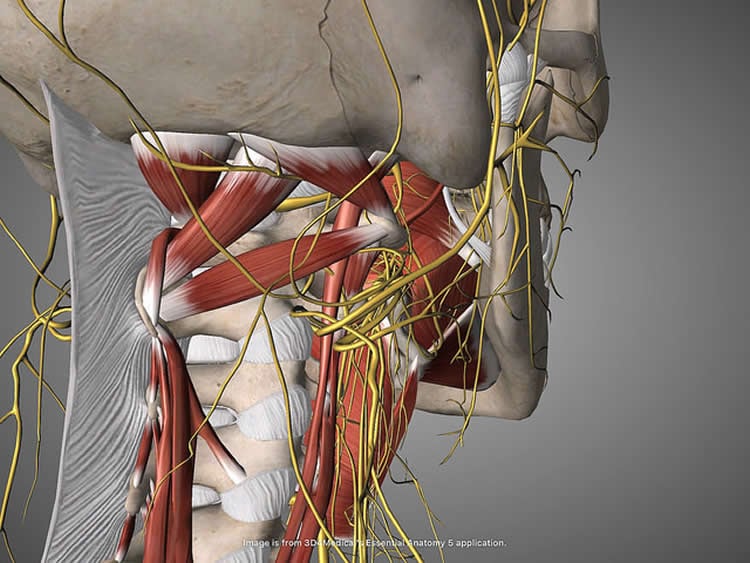
Parkinson’s disease may start in the gut and spread to the brain via the vagus nerve, according to a study published in the April 26, 2017, online issue of Neurology. The vagus nerve extends from the brainstem to the abdomen and controls unconscious body processes like heart rate and food digestion.
The preliminary study examined people who had resection surgery, removing the main trunk or branches of the vagus nerve. The surgery, called vagotomy, is used for people with ulcers. Researchers used national registers in Sweden to compare 9,430 people who had a vagotomy over a 40-year period to 377,200 people from the general population. During that time, 101 people who had a vagotomy developed Parkinson’s disease, or 1.07 percent, compared to 4,829 people in the control group, or 1.28 percent. This difference was not significant.
But when researchers analyzed the results for the two different types of vagotomy surgery, they found that people who had a truncal vagotomy at least five years earlier were less likely to develop Parkinson’s disease than those who had not had the surgery and had been followed for at least five years. In a truncal vagotomy, the nerve trunk is fully resected. In a selective vagotomy, only some branches of the nerve are resected.
A total of 19 people who had truncal vagotomy at least five years earlier developed the disease, or 0.78 percent, compared to 3,932 people who had no surgery and had been followed for at least five years, at 1.15 percent. By contrast, 60 people who had selective vagotomy five years earlier developed Parkinson’s disease, or 1.08 percent.
After adjusting for factors such as chronic obstructive pulmonary disease, diabetes, arthritis and other conditions, researchers found that people who had a truncal vagotomy at least five years before were 40 percent less likely to develop Parkinson’s disease than those who had not had the surgery and had been followed for at least five years.
“These results provide preliminary evidence that Parkinson’s disease may start in the gut,” said study author Bojing Liu, MSc, of the Karolinska Instituet in Stockholm, Sweden. “Other evidence for this hypothesis is that people with Parkinson’s disease often have gastrointestinal problems such as constipation, that can start decades before they develop the disease. In addition, other studies have shown that people who will later develop Parkinson’s disease have a protein believed to play a key role in Parkinson’s disease in their gut.”
The theory is that these proteins can fold in the wrong way and spread that mistake from cell to cell.
“Much more research is needed to test this theory and to help us understand the role this may play in the development of Parkinson’s,” Liu said. Additionally, since Parkinson’s is a syndrome, there may be multiple causes and pathways.
Even though the study was large, Liu said one limitation was small numbers in certain subgroups. Also, the researchers could not control for all potential factors that could affect the risk of Parkinson’s disease, such as smoking, coffee drinking or genetics.
Funding: The study was supported by the Swedish Research Council for Health, Working Life and Welfare, the Parkinson Research Foundation in Sweden, and the U.S. National Institutes of Health.
Source: Renee Tessman – AAN
Image Source: NeuroscienceNews.com image is credited to Beth Scupham and is licensed CC BY 2.0.
Original Research: Abstract for “Vagotomy and Parkinson disease: A Swedish register–based matched-cohort study” by Bojing Liu, Fang Fang, Nancy L. Pedersen, Annika Tillander, Jonas F. Ludvigsson, Anders Ekbom, Per Svenningsson, Honglei Chen, and Karin Wirdefeldt in Neurology. Published online April 26 2017 doi:10.1212/WNL.0000000000003961
[cbtabs][cbtab title=”MLA”]AAN “Could Parkinson’s Disease Start in the Gut?.” NeuroscienceNews. NeuroscienceNews, 26 April 2017.
<https://neurosciencenews.com/parkinsons-vagotomy-6518/>.[/cbtab][cbtab title=”APA”]AAN (2017, April 26). Could Parkinson’s Disease Start in the Gut?. NeuroscienceNew. Retrieved April 26, 2017 from https://neurosciencenews.com/parkinsons-vagotomy-6518/[/cbtab][cbtab title=”Chicago”]AAN “Could Parkinson’s Disease Start in the Gut?.” https://neurosciencenews.com/parkinsons-vagotomy-6518/ (accessed April 26, 2017).[/cbtab][/cbtabs]
Abstract
Vagotomy and Parkinson disease: A Swedish register–based matched-cohort study
Objective: To examine whether vagotomy decreases the risk of Parkinson disease (PD).
Methods: Using data from nationwide Swedish registers, we conducted a matched-cohort study of 9,430 vagotomized patients (3,445 truncal and 5,978 selective) identified between 1970 and 2010 and 377,200 reference individuals from the general population individually matched to vagotomized patients by sex and year of birth with a 40:1 ratio. Participants were followed up from the date of vagotomy until PD diagnosis, death, emigration out of Sweden, or December 31, 2010, whichever occurred first. Vagotomy and PD were identified from the Swedish Patient Register. We estimated hazard ratios (HRs) with 95% confidence intervals (CIs) using Cox models stratified by matching variables, adjusting for country of birth, chronic obstructive pulmonary disease, diabetes mellitus, vascular diseases, rheumatologic disease, osteoarthritis, and comorbidity index.
Results: A total of 4,930 cases of incident PD were identified during 7.3 million person-years of follow-up. PD incidence (per 100,000 person-years) was 61.8 among vagotomized patients (80.4 for truncal and 55.1 for selective) and 67.5 among reference individuals. Overall, vagotomy was not associated with PD risk (HR 0.96, 95% CI 0.78–1.17). However, there was a suggestion of lower risk among patients with truncal vagotomy (HR 0.78, 95% CI 0.55–1.09), which may be driven by truncal vagotomy at least 5 years before PD diagnosis (HR 0.59, 95% CI 0.37–0.93). Selective vagotomy was not related to PD risk in any analyses.
Conclusions: Although overall vagotomy was not associated the risk of PD, we found suggestive evidence for a potential protective effect of truncal, but not selective, vagotomy against PD development.
“Vagotomy and Parkinson disease: A Swedish register–based matched-cohort study” by Bojing Liu, Fang Fang, Nancy L. Pedersen, Annika Tillander, Jonas F. Ludvigsson, Anders Ekbom, Per Svenningsson, Honglei Chen, and Karin Wirdefeldt in Neurology. Published online April 26 2017 doi:10.1212/WNL.0000000000003961






