Summary: Study reveals 412 counties, mainly in the Midwest and South, are at the highest risk of opioid deaths in the US. Researchers propose new strategies for improving treatment for opioid addiction.
Source: University of Michigan
Dozens of counties in the Midwest and South are at the highest risk for opioid deaths in the United States, say University of Michigan researchers.
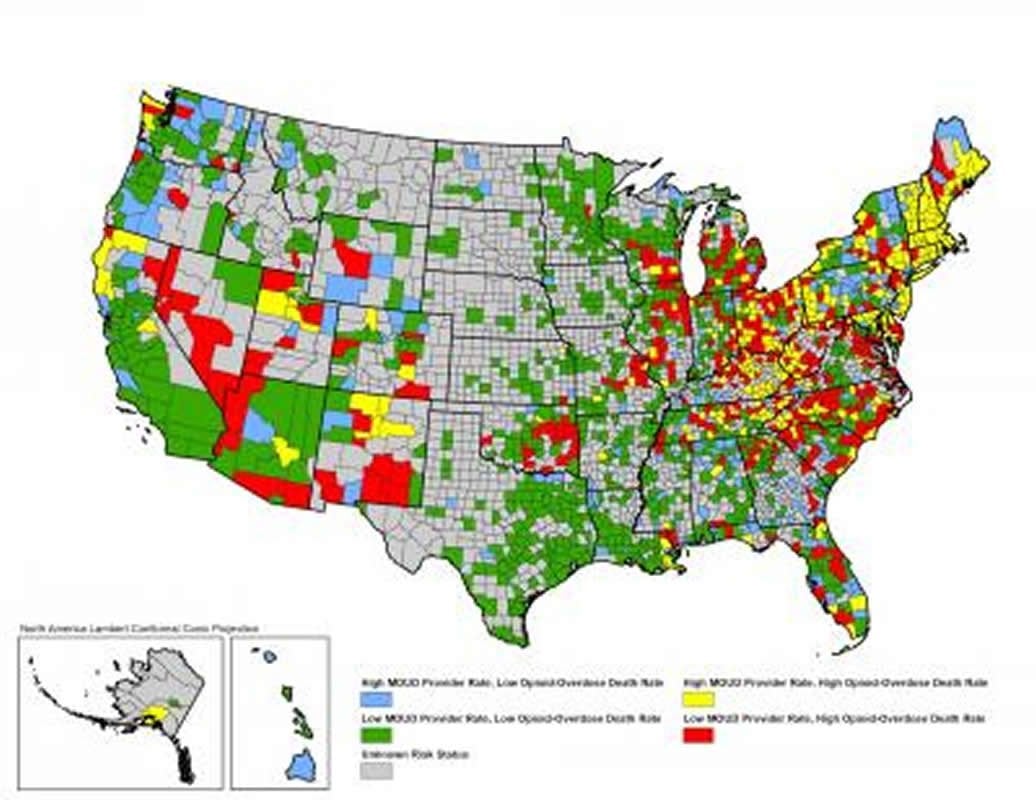
In a study of more than 3,000 counties across the U.S., the researchers found that residents of 412 counties are at least twice as likely to be at high risk for opioid overdose deaths and to lack providers who can deliver medications to treat opioid use disorder.
States with among the most high-risk counties include North Carolina, Ohio, Virginia, Kentucky, Michigan, Tennessee, Illinois, Indiana, Georgia, Oklahoma, West Virginia, South Carolina, Wisconsin and Florida.
The study, published in the June 28 issue of JAMA Network Open, suggests strategies for increasing treatment for opioid addiction, including by increasing the number of primary care clinicians capable of providing medications as well as improving employment opportunities in those communities.
“We hope policymakers can use this information to funnel additional money and resources to specific counties within their states,” said lead author Rebecca Haffajee, assistant professor of health management and policy at the U-M School of Public Health.
“We need more strategies to augment and increase the primary care provider workforce in those high-risk counties, people who are willing and able to provide opioid use disorder treatments.”
The U-M researchers looked at opioid overdose mortality rates in 3,142 U.S. counties between January 2015 and December 2017. They defined an opioid high-risk county as one with opioid overdose mortality above the national rate and with the availability of providers to deliver opioid use disorder medications below the national rate.
The study, they say, is the first to include data from all three opioid use disorder medications on the market, including methadone, buprenorphine and naltrexone. Their analysis included publicly listed providers of methadone (1,517 opioid treatment programs), buprenorphine (24,851 clinicians approved to prescribe the medication) and the extended-release naltrexone product Vivitrol (5,222 health care providers, as compiled by the drug manufacturer).
In their cross-sectional study, the researchers also looked at demographics, workforce, access to health care insurance, road density, urbanicity and opioid prescriptions.
Among counties analyzed, they found that:
- 412 counties (13%) are classified as high-risk, having both high opioid overdose mortality and low treatment capacity.
- 751 counties (24%) had a high rate of opioid overdose mortality.
- 1,457 (46%) counties lacked a publicly available provider of opioid use disorder medication.
- 946 out of 1,328 rural counties (71%) lacked a publicly available provider of opioid use disorder medication.
The study found that certain factors–such as a younger population, lower rates of unemployment and higher density of primary care physicians–are associated with a lower risk of opioid overdose death and lack of capacity to treat opioid use disorder.
Haffajee, also a member of the U-M Institute for Healthcare Policy and Innovation, said it’s important to understand the differences of the opioid epidemic at the local level.
“In rural areas, the opioid crisis is often still a prescription opioid issue. But in metropolitan counties, highly potent illicit fentanyl and other synthetic opioids are more prevalent and are killing people,” she said. “That’s likely why we identified metropolitan areas as higher-risk, despite the fact that these counties typically have some (just not enough) treatment providers.
“Understanding these differences at the sub-state level and coming up with strategies that target specific county needs can allow us to more efficiently channel the limited amount of resources we have to combat this crisis.”
In addition to Haffajee, authors included Lewei Allison Lin, assistant professor of psychiatry; Amy Bohnert, associate professor of medicine; and Jason Goldstick, research assistant professor of emergency medicine. All are part of the Opioid Solutions Network at U-M.
Source:
University of Michigan
Media Contacts:
Nardy Baeza Bickel – University of Michigan
Image Source:
The image is credited to Rebecca L. Haffajee, JD, PhD, MPH; Lewei Allison Lin, MD, MS; Amy S. B. Bohnert, PhD, MHS; Jason E. Goldstick, PhD.
Original Research: Open access
“Characteristics of US Counties With High Opioid Overdose Mortality and Low Capacity to Deliver Medications for Opioid Use Disorder”. Rebecca L. Haffajee, JD, PhD, MPH; Lewei Allison Lin, MD, MS; Amy S. B. Bohnert, PhD, MHS; Jason E. Goldstick, PhD.
JAMA Network Open. doi:10.1001/jamanetworkopen.2019.6373
Abstract
Characteristics of US Counties With High Opioid Overdose Mortality and Low Capacity to Deliver Medications for Opioid Use Disorder
Importance
Opioid overdose deaths in the United States continue to increase, reflecting a growing need to treat those with opioid use disorder (OUD). Little is known about counties with high rates of opioid overdose mortality but low availability of OUD treatment.
Objective
To identify characteristics of US counties with persistently high rates of opioid overdose mortality and low capacity to deliver OUD medications.
Design, Setting, and Participants
In this cross-sectional study of data from 3142 US counties from January 1, 2015, to December 31, 2017, rates of opioid overdose mortality were compared with availability in 2017 of OUD medication providers (24 851 buprenorphine-waivered clinicians [physicians, nurse practitioners, and physician assistants], 1517 opioid treatment programs [providing methadone], and 5222 health care professionals who could prescribe extended-release naltrexone). Statistical analysis was performed from April 20, 2018, to May 8, 2019.
Exposures
Demographic, workforce, lack of insurance, road density, urbanicity, opioid prescribing, and regional division county-level characteristics.
Main Outcome and Measures
The outcome variable, “opioid high-risk county,” was a binary indicator of a high (above national) rate of opioid overdose mortality with a low (below national) rate of provider availability to deliver OUD medication. Spatial logistic regression models were used to determine associations with being an opioid high-risk county.
Results
Of 3142 counties, 751 (23.9%) had high rates of opioid overdose mortality. A total of 1457 counties (46.4%), and 946 of 1328 rural counties (71.2%), lacked a publicly available OUD medication provider in 2017. In adjusted models, compared with the West North Central division, counties in the East North Central, Mountain, and South Atlantic divisions had increased odds of being opioid high-risk counties (East North Central: odds ratio [OR], 2.21; 95% CI, 1.19-4.12; Mountain: OR, 4.15; 95% CI, 1.34-12.89; and South Atlantic: OR, 2.99; 95% CI, 1.26-7.11). A 1% increase in unemployment was associated with increased odds (OR, 1.09; 95% CI, 1.03-1.15) of a county being an opioid high-risk county. Counties with an additional 10 primary care clinicians per 100 000 population had a reduced risk of being opioid high-risk counties (OR, 0.89; 95% CI, 0.85-0.93), as did counties that were micropolitan (vs metropolitan) (OR, 0.67; 95% CI, 0.50-0.90) and those that had an additional 1% of the population younger than 25 years (OR, 0.95; 95% CI, 0.92-0.98).
Conclusions and Relevance
Counties with low availability of OUD medication providers and high rates of opioid overdose mortality were less likely to be micropolitan and have lower primary care clinician density, but were more likely to be in the East North Central, South Atlantic, or Mountain division and have higher rates of unemployment. Strategies to increase medication treatment must account for these factors.






