Summary: Researchers have developed a promising CAR-T cell therapy targeting glioblastoma, the most aggressive brain tumor. The therapy uses genetically modified T cells to target a specific marker on tumor cells, potentially overcoming the limitations of traditional treatments.
Notably, these CAR-T cells also show an ability to fight tumor cells lacking the marker, suggesting a bystander effect. Early trials in mice demonstrate that this approach effectively controls tumor growth with minimal toxicity, setting the stage for human clinical trials.
Key Facts:
- CAR-T therapy targets glioblastoma, a highly aggressive brain tumor.
- The therapy shows a “bystander effect,” attacking tumor cells without the target marker.
- In mouse models, it prolonged survival without significant toxicity, promising safer treatments.
Source: University of Geneva
Glioblastoma is the most common and most aggressive primary brain tumour, with an average survival after diagnosis of less than two years, and against which current treatments remain ineffective. In recent years, immunotherapies have given patients renewed hope, albeit with relatively modest success.
A team from the University of Geneva (UNIGE) and the Geneva University Hospitals (HUG) has succeeded in identifying a specific marker on the surface of tumour cells, and in generating immune cells carrying an antibody to destroy them.
Furthermore, these cells, called CAR-T cells, appear to be capable of targeting diseased cells in the tumour that do not carry this antigen, while sparing healthy cells.
These results, published in the journal Cancer Immunology Research, are a first step towards the development of clinical trials with human patients.
Glioblastomas carry biological characteristics that make them particularly difficult to treat. Able to induce a microenvironment that limits the attack of the immune system, they escape standard treatments and recur rapidly.
Denis Migliorini, assistant professor in the Department of Medicine at the UNIGE Faculty of Medicine, holder of the ISREC Foundation Chair in Brain Tumour Immunology, member of the Translational Research Centre in Onco-Haematology (CRTOH) and attending physician in charge of the HUG Neuro-oncology Unit, is an expert in CAR-T cells (for chimeric antigen receptors T-cells).
This immunotherapy consists in collecting immune T cells from patients, modifying them genetically in the lab to make them express antibodies capable of detecting elements specific to tumour cells, before reinjecting them so that they can specifically target the tumour.
‘‘For several years we have been trying to identify the protein markers expressed by glioblastoma cells,’’ explains Denis Migliorini.
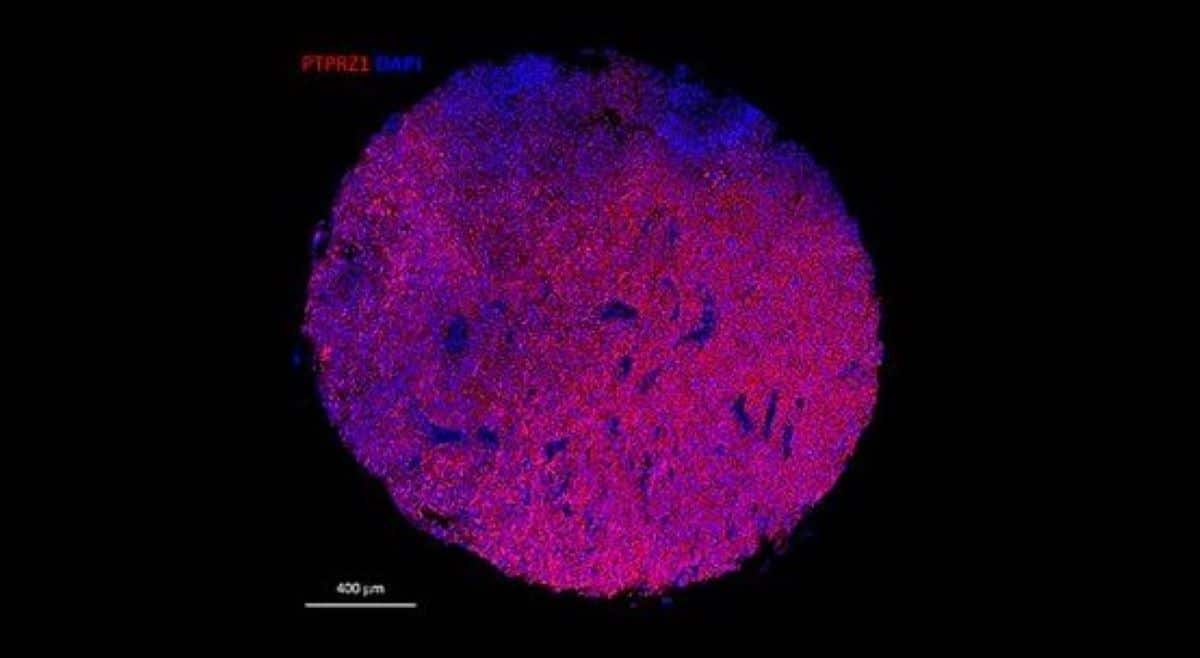
‘‘One of these markers, PTPRZ1, proved particularly important: we were able to generate CAR-T cells carrying antibodies targeting PTPRZ1. This is a first step towards CAR-T cells effective against malignant gliomas.”
mRNA to make a customised cell
Most CAR-T cells are generated using viral vectors, a technique that has proved its worth in certain diseases but is not very suitable in the brain.
‘‘Indeed, they persist for a very long time in the context blood cancers. The brain is a fragile organ, and this persistence can generate a risk of toxicity,’’ explains Darel Martinez Bedoya, a post-doctoral fellow in Denis Migliorini’s laboratory and first author of this research.
The scientists therefore introduced in the T-cells the messenger RNA encoding for the desired antibody. The cellular machinery is then responsible for producing the right protein to build the receptor that will take place on the T-cell surface and recognise the tumour target.
‘‘This technique has a number of advantages: CAR-Ts offer a flexible platform, allowing multiple adaptations according to the specificities and evolution of the tumour,’’ explains Darel Martinez Bedoya.
Efficacy and safety
To check that CAR-Ts only attack tumour cells, the Geneva team first tested them in vitro on healthy and tumour cells.
‘‘To our surprise, not only did CAR-Ts not attack healthy cells, but they were also capable, by bystander effect, of identifying and fighting tumour cells not expressing the PTPRZ1 marker,’’ Denis Migliorini is delighted to report.
‘‘In this context, CAR-Ts are probably capable of secreting pro-inflammatory molecules that are responsible for eliminating tumour cells even in the absence of the original marker when co-cultured with target positive tumour cells.’’
The second stage involved testing the treatment in vivo in mouse models of human glioblastoma. Tumour growth was controlled, prolonging the lives of the mice remarkably well without signs of toxicity.
‘‘By administering CAR-Ts intratumourally in the CNS, we can use fewer cells and greatly reduce the risk of peripheral toxicity. With this data and other unpublished yet, all lights are green to now envisage a first clinical trial in humans,’’ the scientists conclude.
About this glioblastoma brain cancer research news
Author: Antoine Guenot
Source: University of Geneva
Contact: Antoine Guenot – University of Geneva
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“PTPRZ1-targeting RNA CAR T cells exert antigen-specific and bystander antitumor activity in glioblastoma” by Denis Migliorini et al. Cancer Immunology Research
Abstract
PTPRZ1-targeting RNA CAR T cells exert antigen-specific and bystander antitumor activity in glioblastoma
The great success of chimeric antigen receptor (CAR) T-cell therapy in the treatment of patients with B-cell malignancies has prompted its translation to solid tumors.
In the case of glioblastoma (GBM), clinical trials have shown modest efficacy, but efforts to develop more effective anti-GBM CAR T cells are ongoing. In this study, we selected PTPRZ1 as a target for GBM treatment.
We isolated six anti-human PTPRZ1 scFv from a human phage display library and produced 2nd generation CAR T cells in an RNA format.
Patient-derived GBM PTPRZ1-knock-in cell lines were used to select the CAR construct that showed high cytotoxicity while consistently displaying high CAR expression (471_28z).
CAR T cells incorporating 471_28z were able to release IFN-γ, IL-2, TNF-α, Granzyme B, IL-17A, IL-6, and soluble FasL, and displayed low tonic signaling. Additionally, they maintained an effector memory phenotype after in vitro killing.
In addition, 471_28z CAR T cells displayed strong bystander killing against PTPRZ1-negative cell lines after pre-activation by PTPRZ1-positive tumor cells but did not kill antigen-negative non-tumor cells.
In an orthotopic xenograft tumor model using NSG mice, a single dose of anti-PTPRZ1 CAR T cells significantly delayed tumor growth.
Taken together, these results validate PTPRZ1 as a GBM target and prompt the clinical translation of anti-PTPRZ1 CAR T cells.






