Summary: Researchers have discovered a way to control human body temperature, mimicking the hibernation process of animals like bears. By manipulating the brain’s temperature regulation system, they can induce a state of “thermoregulatory inversion” (TI) in rats, reducing heat production even in cold environments.
This breakthrough could lead to controlled hypothermia in humans, improving survival rates in life-threatening situations like heart attacks and strokes. The discovery opens the door to therapeutic hypothermia, which can protect tissues from damage by lowering metabolism and oxygen demand.
Key Facts:
- Thermoregulatory Inversion (TI): A new process that reduces heat production in response to cold.
- Brain Mechanism: The ventromedial periventricular area (VMPeA) controls the TI state.
- Human Application: TI could help manage ischemia during surgeries, metabolic disorders, and brain injuries.
Source: Oregon Health and Science University
In the same way a bear instinctively lowers its body temperature to survive the winter’s chill, scientists have discovered a groundbreaking method to control human body temperature —potentially saving lives in emergency situations.
Oregon Health & Science University researchers have identified a process that could one day help clinicians lower body temperature in people experiencing life-threatening events, such as heart attacks or strokes.
Video Credit: Neuroscience News
If applied in humans, who can’t naturally hibernate, the discovery could mimic the natural ability of certain animals to lower their body temperature during hibernation.
“The idea is to reduce the body temperature to a lower level so that tissues like the brain or heart don’t need as much oxygen, allowing them to survive the ischemia [lack of oxygen to tissues] longer and improve the functional outcomes of strokes or heart attacks,” said Domenico Tupone, Ph.D., senior author of the study and research assistant professor of neurological surgery in the OHSU School of Medicine.
Normally, when mammals get cold, their bodies try to generate heat by shivering or burning a special kind of fat called brown fat. This is controlled by the brain’s normal thermoregulation system, which keeps the body temperature stable.
However, in hibernating animals, like bears or Arctic ground squirrels, this system gets altered during the winter so they can lower their body temperature and survive the cold for long periods.
During the hibernation process, or torpor, the body’s usual responses to cold exposure are inverted so that cold exposure causes the reduction of heat generation and body temperature drops.
In their study, published today in the journal Current Biology, Tupone and colleagues discovered how the brain controls this change in temperature regulation. They call this process “thermoregulatory inversion” or TI.
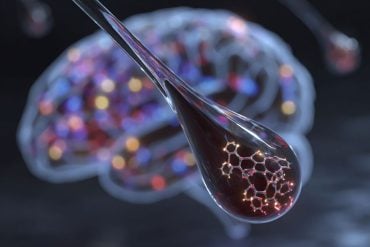
The researchers found that by blocking a certain area in the brain, called the ventromedial periventricular area, or VMPeA, they could trigger this TI state in rats — animals that, like humans, don’t hibernate naturally.
During TI, exposure to cold environments stops the body from producing heat, a process known as thermogenesis, while exposure to warm increases heat production.
Their research reveals that the VMPeA acts as a “torpor switch”: When it’s active, the body reacts normally to temperature changes. However, when the activity in this part of the brain is reduced, the body shifts into TI, lowering heat production, even in the cold. This discovery could lead to controlled hypothermia in humans.

“If we had a mechanism that allows us to transform humans into hibernating animals, we could achieve and control therapeutic hypothermia much better,” Tupone said.
By inducing the TI state in rats, these researchers showed it is possible to create a controlled hypothermia in animals that don’t hibernate. This could be useful in human medicine, such as during surgeries, for treating metabolic disorders or for managing brain injuries.
Lowering body temperature in these situations can reduce tissue damage and improve recovery. The goal is to induce a low temperature, low metabolism state — therapeutic hypothermia — to give patients a better chance of surviving tissue ischemia, during long surgeries, or even on long space missions.
In addition to Tupone, co-authors include: Shaun Morrison, Ph.D., and Pierfrancesco Chiavetta, M.D., of OHSU; and Georgina Cano, Ph.D., and Shelby Hernan, Ph.D., of the University of Pittsburgh.
Funding: This research was supported by the National Institutes of Health’s, National Institute of Neurological Disorders and Stroke under Award Numbers R01NS099234 and R01NS091066 and Office of the Director under Award Number P40OD010996.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
All research involving animal subjects at OHSU must be reviewed and approved by the university’s Institutional Animal Care and Use Committee (IACUC). The IACUC’s priority is to ensure the health and safety of animal research subjects.
The IACUC also reviews procedures to ensure the health and safety of the people who work with the animals. The IACUC conducts a rigorous review of all animal research proposals to ensure they demonstrate scientific value and justify the use of live animals.
About this thermoregulation and neuroscience research news
Author: Angela Yeager
Source: Oregon Health and Science University
Contact: Angela Yeager – Oregon Health and Science University
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Inhibition of the hypothalamic ventromedial periventricular area activates a dynorphin pathway-dependent thermoregulatory inversion in rats” by Domenico Tupone et al. Current Biology
Abstract
Inhibition of the hypothalamic ventromedial periventricular area activates a dynorphin pathway-dependent thermoregulatory inversion in rats
To maintain core body temperature in mammals, CNS thermoregulatory networks respond to cold exposure by increasing brown adipose tissue and shivering thermogenesis.
However, in hibernation or torpor, this canonical thermoregulatory response is replaced by a new, emerging paradigm, thermoregulatory inversion (TI), an alternative homeostatic state in which cold exposure inhibits thermogenesis and warm exposure stimulates thermogenesis.
Here, we demonstrate that in the non-torpid rat, either exclusion of the canonical thermoregulatory integrator in the preoptic hypothalamus or inhibition of neurons in the ventromedial periventricular area (VMPeA) induces the TI state through an alternative thermoregulatory pathway.
Within this pathway, we have identified a dynorphinergic input to the dorsomedial hypothalamus from the dorsolateral parabrachial nucleus that plays a critical role in mediating the cold-evoked inhibition of thermogenesis during TI.
Our results reveal a novel thermosensory reflex circuit within the mammalian CNS thermoregulatory pathways and support the potential for pharmacologically inducing the TI state to elicit therapeutic hypothermia in non-hibernating species, including humans.