Summary: Pain could be an under-recognized clinical manifestation for patients with specific autoantibodies that target neural proteins.
Source: University of Oxford
In a new study, four research groups within the Department combine their strengths in autoimmunity, pain and peripheral nerve diseases.
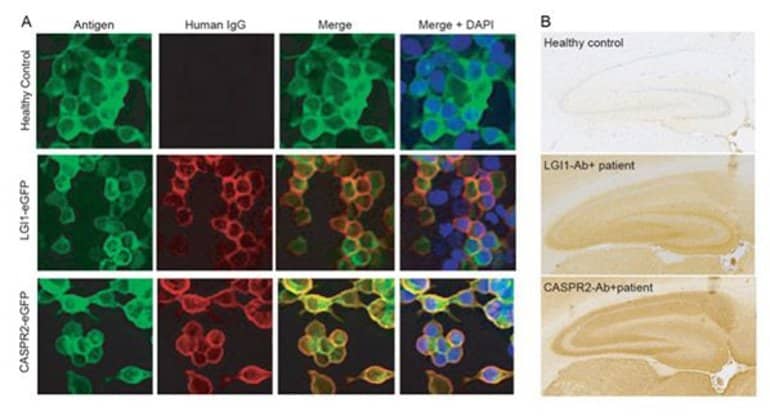
Their collective findings reveal that patients with antibodies to LGI1 and CASPR2 show different clinical, immunological and neurobiological characteristics which may relate to the antibodies differentially targeting neurons which can mediate pain.
The findings have implications for improving the long-term outcomes of these patients and for our understanding of the basic biology of these antigenic targets.
About this pain research news
Author: Press Office
Source: University of Oxford
Contact: Press Office – University of Oxford
Image: The image is credited to the researchers
Original Research: Open access.
“Leucine-Rich Glioma-Inactivated 1 versus Contactin-Associated Protein-like 2 Antibody Neuropathic Pain: Clinical and Biological Comparisons” by Irani et al. Annals of Neurology
Abstract
Leucine-Rich Glioma-Inactivated 1 versus Contactin-Associated Protein-like 2 Antibody Neuropathic Pain: Clinical and Biological Comparisons
Pain is a under-recognized association of leucine-rich glioma-inactivated 1 (LGI1) and contactin-associated protein-like 2 (CASPR2) antibodies. Of 147 patients with these autoantibodies, pain was experienced by 17 of 33 (52%) with CASPR2- versus 20 of 108 (19%) with LGI1 antibodies (p = 0.0005), and identified as neuropathic in 89% versus 58% of these, respectively.
Typically, in both cohorts, normal nerve conduction studies and reduced intraepidermal nerve fiber densities were observed in the sampled patient subsets. In LGI1 antibody patients, pain responded to immunotherapy (p = 0.008), often rapidly, with greater residual patient-rated impairment observed in CASPR2 antibody patients (p = 0.019).
Serum CASPR2 antibodies, but not LGI1 antibodies, bound in vitro to unmyelinated human sensory neurons and rodent dorsal root ganglia, suggesting pathophysiological differences that may underlie our clinical observations.






