Summary: In patients with ALS, astrocytes within the brain become pro-inflammatory and tend to lose their protective function, resulting in changes in the ability to uptake glutamate.
Source: Francis Crick Institute
Scientists at the Francis Crick Institute have revealed harmful changes in supporting cells, called astrocytes, in Amyotrophic Lateral Sclerosis (ALS) in two publications in Brain and Genome Research.
ALS, also known as motor neuron disease, is a rapidly progressing degenerative disease of the nervous system, meaning patients suffer loss of strength, speech and eventually the ability to breathe. There are currently no effective treatments and tragically most people die within 3 to 5 years.
When healthy, astrocytes help protect and nurture surrounding motor neurons. However, while recent findings from ALS patients have indicated astrocytes may contribute to the disease, how they go about this remains unclear.
Toxic astrocyte changes in ALS
In the first paper, published in Genome Research (in December), the researchers analysed all existing public datasets of astrocytes in ALS, spanning both human and mouse models. Using this meta-analysis approach, they found that in ALS, astrocytes become pro-inflammatory, which is toxic to neighbouring motor neurons.
ALS astrocytes were also found to lose important protective functions, notably the ability to uptake a substance called glutamate. This leads to a build-up of glutamate, which damages motor neurons.
Oliver Ziff, study lead and clinical fellow in the Crick’s Human Stem Cells and Neurodegeneration Laboratory, said: “Our work suggests that treatments for ALS will need to reduce or reverse these damaging changes in astrocytes. These cells are not just innocent bystanders but actively contribute to the progression of the disease.”
Innate and diverse harmful changes in ALS astrocytes
In the second study, published in Brain today (19 January), the researchers found that astrocytes with different ALS-causing genetic mutations also have distinct underlying molecular patterns. This suggests that, during ALS, astrocytes acquire mutation-dependent changes.
As part of their study, the team examined the impact of different mutations known to cause ALS on astrocytes. They observed that in the absence of any neighbouring immune cells, such as microglia, the presence of these mutations alone was sufficient to drive harmful changes in the astrocytes.
The nature of these changes depended on the specific mutations present, suggesting that astrocytes in ALS can appear diverse between different patients. The researchers observed key molecular and functional differences in the cells as a result of the mutation they carried.
However, they also showed that some of these changes converge, which might explain why, in disease, astrocytes have similar characteristics, failing to protect motor neurons from degeneration and increasing inflammation that in turn drives disease.

Doaa Taha, study lead, co-lead author on the first paper and UCL PhD student in the Crick’s Human Stem Cells and Neurodegeneration Laboratory, said: “The nature and diversity of astrocyte transformation between ALS mutations was not well known. The insight we’ve gained into the different ways this change manifests in early disease could be a helpful starting point in efforts to reverse the cell transformation.”
Ben Clarke, co-lead author on both papers and postdoc in the Human Stem Cells and Neurodegeneration Laboratory, said: “We’re now working to understand the biology of the distinct molecular patterns we’re observing and how they converge. Understanding the early astrocyte changes in ALS could provide us with new therapeutic targets.”
Growing models
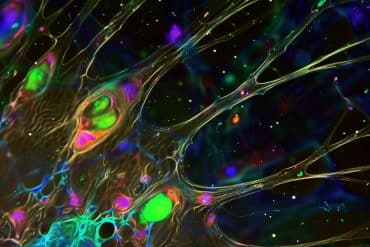
While much research into ALS relies on post-mortem samples, where the disease is already well-established, these studies involve growing living cells derived from patients. Master stem cells can be taught to differentiate into any cell from anywhere in the human body, meaning scientists can observe the very earliest cell changes caused by different genetic mutations. The Patani Lab at the Francis Crick Institute are leaders in growing astrocytes and other cells of the nervous system from human induced pluripotent stem cells.
“Our growing understanding of early disease biology is bringing us closer to finding new ways to treat ALS,” says Rickie Patani, head of the Crick’s Human Stem Cells and Neurodegeneration Laboratory, Consultant Neurologist at the National Hospital for Neurology and Neurosurgery and member of the UCL Queen Square Motor Neuron Disease Centre. “It’s at the origin of these ‘star’ cells that we might uncover crucial changes that drive the disease.”
About this ALS research news
Author: Alice Deeley
Source: Francis Crick Institute
Contact: Alice Deeley – Francis Crick Institute
Original Research: Open access.
“Astrocytes display cell autonomous and diverse early reactive states in familial amyotrophic lateral sclerosis” by Doaa Taha et al. Brain
Closed access.
“Meta-analysis of human and mouse ALS astrocytes reveals multi-omic signatures of inflammatory reactive states” by Oliver Ziff et al. Genome Research
Abstract
Astrocytes display cell autonomous and diverse early reactive states in familial amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis is a rapidly progressive and fatal disease. Although astrocytes are increasingly recognized contributors to the underlying pathogenesis, the cellular autonomy and uniformity of astrocyte reactive transformation in different genetic forms of amyotrophic lateral sclerosis remain unresolved.
Here we systematically examine these issues by using highly enriched and human induced pluripotent stem cell-derived astrocytes from patients with VCP and SOD1 mutations.
We show that VCP mutant astrocytes undergo cell-autonomous reactive transformation characterized by increased expression of complement component 3 (C3) in addition to several characteristic gene expression changes. We then demonstrate that isochronic SOD1 mutant astrocytes also undergo a cell-autonomous reactive transformation, but that this is molecularly distinct from VCP mutant astrocytes.
This is shown through transcriptome-wide analyses, identifying divergent gene expression profiles and activation of different key transcription factors in SOD1 and VCP mutant human induced pluripotent stem cell-derived astrocytes. Finally, we show functional differences in the basal cytokine secretome between VCP and SOD1 mutant human induced pluripotent stem cell-derived astrocytes.
Our data therefore reveal that reactive transformation can occur cell autonomously in human amyotrophic lateral sclerosis astrocytes and with a striking degree of early molecular and functional heterogeneity when comparing different disease-causing mutations. These insights may be important when considering astrocyte reactivity as a putative therapeutic target in familial amyotrophic lateral sclerosis.
Abstract
Meta-analysis of human and mouse ALS astrocytes reveals multi-omic signatures of inflammatory reactive states
Astrocytes contribute to motor neuron death in amyotrophic lateral sclerosis (ALS), but whether they adopt deleterious features consistent with inflammatory reactive states remains incompletely resolved.
To identify inflammatory reactive features in ALS human induced pluripotent stem cell (hiPSC)–derived astrocytes, we examined transcriptomics, proteomics, and glutamate uptake in VCP-mutant astrocytes.
We complemented this by examining other ALS mutations and models using a systematic meta-analysis of all publicly-available ALS astrocyte sequencing data, which included hiPSC-derived astrocytes carrying SOD1, C9orf72, and FUS gene mutations as well as mouse ALS astrocyte models with SOD1G93A mutation, Tardbp deletion, and Tmem259 (also known as membralin) deletion. ALS astrocytes were characterized by up-regulation of genes involved in the extracellular matrix, endoplasmic reticulum stress, and the immune response and down-regulation of synaptic integrity, glutamate uptake, and other neuronal support processes.
We identify activation of the TGFB, Wnt, and hypoxia signaling pathways in both hiPSC and mouse ALS astrocytes. ALS changes positively correlate with TNF, IL1A, and complement pathway component C1q-treated inflammatory reactive astrocytes, with significant overlap of differentially expressed genes. By contrasting ALS changes with models of protective reactive astrocytes, including middle cerebral artery occlusion and spinal cord injury, we uncover a cluster of genes changing in opposing directions, which may represent down-regulated homeostatic genes and up-regulated deleterious genes in ALS astrocytes.
These observations indicate that ALS astrocytes augment inflammatory processes while concomitantly suppressing neuronal supporting mechanisms, thus resembling inflammatory reactive states and offering potential therapeutic targets.