Summary: Scientists have developed a novel surgical method allowing two retinal tissue grafts to be implanted in a single eye, advancing treatment strategies for dry age-related macular degeneration (AMD). This new approach enables side-by-side testing of grafts—one with retinal pigment epithelial (RPE) cells and one without—within the same lesion, using a specially designed clamp to maintain eye pressure and reduce damage.
In animal models, the RPE grafts significantly preserved light-sensing photoreceptors and regenerated the choriocapillaris, the blood vessel layer essential for retinal health. These results enhance ongoing efforts to translate lab-grown stem cell therapies into clinical treatments for vision loss.
Key Facts:
- Dual Grafting Innovation: A new technique allows simultaneous implantation of two grafts for better comparative analysis.
- Photoreceptor Preservation: Grafts containing RPE cells protected light-sensing neurons better than controls.
- Vessel Regeneration: RPE grafts uniquely regenerated the choriocapillaris, crucial for retinal support.
Source: NIH
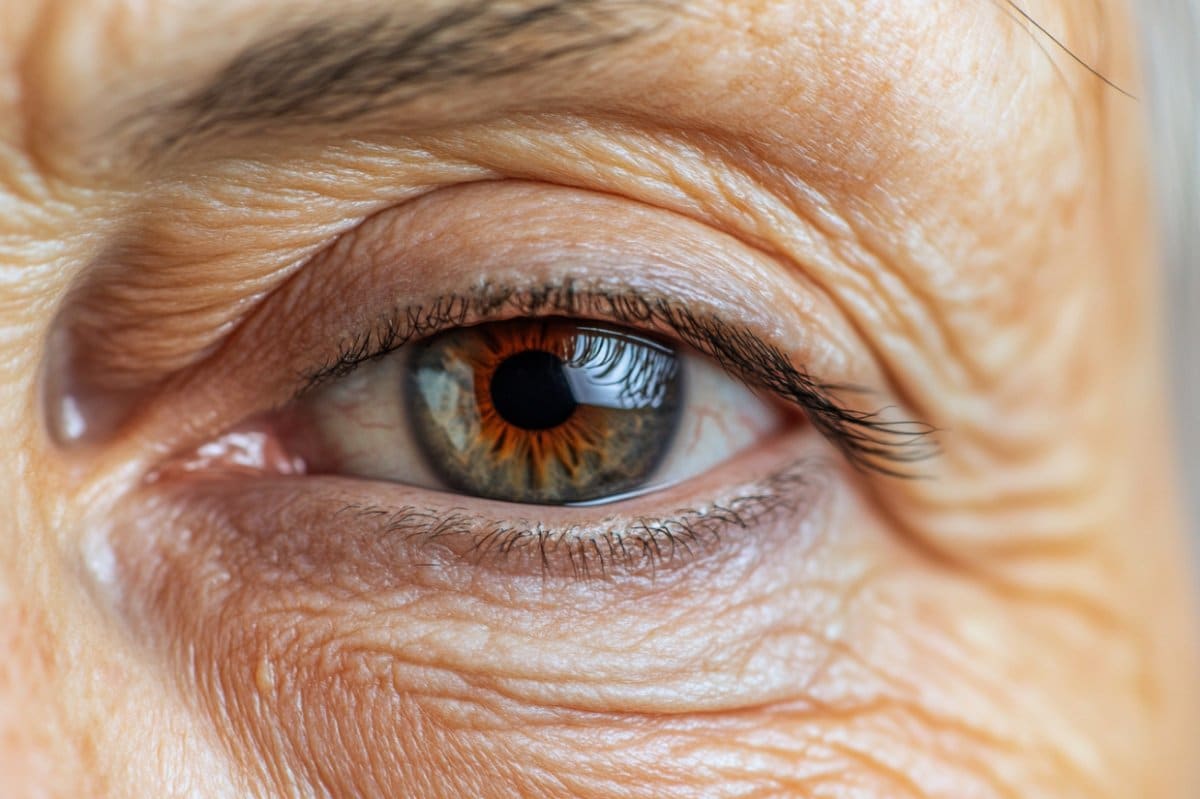
National Institutes of Health (NIH) scientists have developed a new surgical technique for implanting multiple tissue grafts in the eye’s retina.
The findings in animals may help advance treatment options for dry age-related macular degeneration (AMD), which is a leading cause of vision loss among older Americans.
A report about the technique published today in JCI Insight.
Credit: Neuroscience News
In diseases such as AMD, the light-sensitive retina tissue at the back of the eye degenerates. Scientists are testing therapies for restoring damaged retinas with grafts of tissue grown in the lab from patient-derived stem cells.
Until now, surgeons have only been able to place one graft in the retina, limiting the area that can be treated in patients, and as well as the ability to conduct side-by-side comparisons in animal models.
Such comparisons are crucial for confirming that the tissue grafts are integrating with the retina and the underlying blood supply from a network of tiny blood vessels known as the choriocapillaris.
For the technique, investigators designed a new surgical clamp that maintains eye pressure during the insertion of two tissue patches in immediate succession while minimizing damage to the surrounding tissue.
In animal models, the scientists used their newly designed surgical technique to compare two different grafts placed sequentially in the same experimentally induced AMD-like lesion. One graft consisted of retinal pigment epithelial (RPE) cells grown on a biodegradable scaffold. RPE cells support and nourish the retina’s light-sensing photoreceptors.
In AMD, vision loss occurs alongside the loss of RPE cells and photoreceptors. In the lab, RPE cells are grown from human blood cells after they’ve been converted into stem cells. The second graft consisted of just the biodegradable scaffold to serve as a control.
Post surgery, scientists used artificial intelligence to analyze retinal images and compare the effects of each graft. They observed that the RPE grafts promoted the survival of photoreceptors, while photoreceptors near scaffold-only grafts died at a much higher rate.
Additionally, they were able to confirm for the first time that the RPE graft also regenerated the choriocapillaris, which supplies the retina with oxygen and nutrients.
The findings expand on the capability demonstrated in an ongoing, NIH-led first-in-human clinical trial of patient-derived RPE grafts for the dry form of AMD.
Funding: The work was supported by the National Eye Institute Intramural Research Program
About this AMD and visual neuroscience research news
Author: NIH Office of Communications
Source: NIH
Contact: NIH Office of Communications – NIH
Image: The image is credited to Neuroscience News
Original Research: Open access.
“iPSC-RPE patch preserves photoreceptors and regenerates choriocapillaris in a pig outer regina degeneration model” by Kapil Bharti et al. JCI Insight
Abstract
iPSC-RPE patch preserves photoreceptors and regenerates choriocapillaris in a pig outer regina degeneration model
Dry age-related macular degeneration (AMD) is a leading cause of untreatable vision loss. In advanced cases, retinal pigment epithelium (RPE) cell loss occurs alongside photoreceptor and choriocapillaris degeneration.
We hypothesized that an RPE-patch would mitigate photoreceptor and choriocapillaris degeneration to restore vision.
An induced pluripotent stem cell–derived RPE (iRPE) patch was developed using a clinically compatible manufacturing process by maturing iRPE cells on a biodegradable poly(lactic-co-glycolic acid) (PLGA) scaffold.
To compare outcomes, we developed a surgical procedure for immediate sequential delivery of PLGA-iRPE and/or PLGA-only patches in the subretinal space of a pig model of laser-induced outer retinal degeneration.
Deep learning algorithm-based optical coherence tomography (OCT) image segmentation verified preservation of the photoreceptors over the areas of PLGA-iRPE–transplanted retina and not in laser-injured or PLGA-only–transplanted retina.
Adaptive optics imaging of individual cone photoreceptors further supported this finding. OCT-angiography revealed choriocapillaris regeneration in PLGA-iRPE– and not in PLGA-only–transplanted retinas.
Our data, obtained using clinically relevant techniques, verified that PLGA-iRPE supports photoreceptor survival and regenerates choriocapillaris in a laser-injured pig retina.
Sequential delivery of two 8 mm2 transplants allows for testing of surgical feasibility and safety of the double dose. This work allows one surgery to treat larger and noncontiguous retinal degeneration areas.