Researchers at Lund University in Sweden have used a completely new preclinical technique and analysis of tissue from patients to show exactly what happens when certain patients with Parkinson’s disease are restored as a result of nerve cell transplants. They have also identified what makes many of the transplant patients develop serious side effects in the form of involuntary movements.
The treatment of Parkinson’s disease has improved over the past few decades. Despite this, the problem of serious side effects remains, caused by both medication and the transplantation of nerve cells.
Parkinson’s disease is associated with a deficit of the nerve cells that produce the neurotransmitter dopamine in the brain. One treatment method is to transplant dopamine-producing cells into the affected part of the brain. Some patients have been completely restored after such a transplant. Others have experienced side effects, involuntary movements known as dyskinesias.
The reason why transplanted patients develop dyskinesias, which is also a common side effect of medication treatment using L-DOPA, has been unknown up to now.
For several years, the Lund researcher Tomas Björklund and his colleagues have been working to develop a completely new technique for studying how the transplanted cells actually function when they are transplanted into a brain affected by Parkinson’s disease. They have placed an artificial receptor on the surface of transplanted cells. A specially designed drug activates the receptor, which controls the cells’ release of dopamine. In animal testing they have now shown that this method can be used to control the transplanted dopamine-producing cells’ activity in the brain. When the dopamine-producing cells are active, the animal is almost completely restored.
“It is like a remote control for the brain. Using this new technique, we can now either close down the transplanted cells completely or increase their activity”, states Tomas Björklund. “Now we can control very closely when and how the cells function when transplanted into the area of the brain affected by the disease.”
Using this new technique, the researchers have identified the exact signalling pathway in the nerve cells that causes the involuntary movements. This is the chain of events: when the researchers activated the dopamine-producing cells via a specific receptor, 5-HT6, which is sensitive to the neurotransmitter serotonin, cyclic AMP increased within the transplanted cells. This in turn caused an abnormal release of dopamine from the cells, which ultimately caused dyskinesia among the animals.
“We have now been able to map exactly what it is that makes nerve cell transplantation effective as a treatment. We have had access to unique patient material from a patient who has had this type of cell transplant and have also found a very high level expression of the receptor that causes the side effects. The discovery is important, as in future clinical treatment using cell transplantation can be carried out with a considerably reduced risk of side effects, and the effect of the treatment can be enhanced.”
“There are advanced plans in many parts of the world to carry out new clinical studies with nerve cell transplants from both foetuses and stem cells against Parkinson’s disease, which means that it’s now more relevant than ever to identify the underlying mechanisms in the brain.”
Source: Cecilia Schubert – Lund University
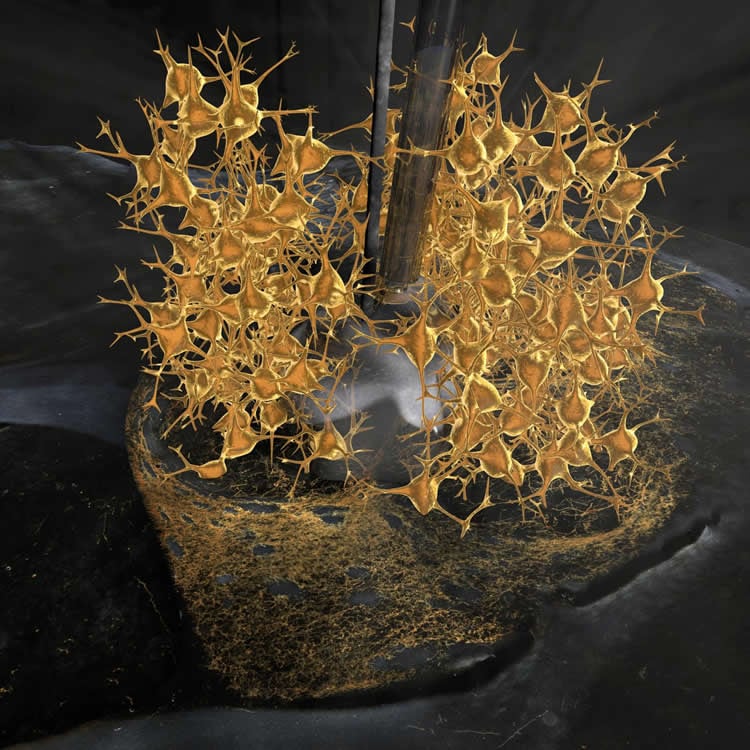
Image Source: The image is credited to Bengt Mattsson.
Original Research: Full open access research for “DREADD modulation of transplanted DA neurons reveals a novel serotonin dependent Parkinsonian dyskinesia mechanism mediated by the 5-HT6 receptor” by Patrick Aldrin-Kirk, Andreas Heuer, Gang Wang, Bengt Mattsson, Martin Lundblad, Malin Parmar, and Tomas Björklund in Neuron. Published online May 5 2016 doi:10.1016/j.neuron.2016.04.017
Abstract
DREADD modulation of transplanted DA neurons reveals a novel serotonin dependent Parkinsonian dyskinesia mechanism mediated by the 5-HT6 receptor
Highlights
•Bimodal DREADDs and transgenic rats enable remote control of transplant function
•Gs-coupled increase of cAMP using DREADDs leads to graft-induced dyskinesias (GIDs)
•Serotonin 5-HT6 receptor stimulation gives GIDs through dysplastic DA release
•DA neurons grafted to the human brain have high levels of the 5-HT6 receptor
Summary
Transplantation of DA neurons is actively pursued as a restorative therapy in Parkinson’s disease (PD). Pioneering clinical trials using transplants of fetal DA neuroblasts have given promising results, although a number of patients have developed graft-induced dyskinesias (GIDs), and the mechanism underlying this troublesome side effect is still unknown. Here we have used a new model where the activity of the transplanted DA neurons can be selectively modulated using a bimodal chemogenetic (DREADD) approach, allowing either enhancement or reduction of the therapeutic effect. We show that exclusive activation of a cAMP-linked (Gs-coupled) DREADD or serotonin 5-HT6 receptor, located on the grafted DA neurons, is sufficient to induce GIDs. These findings establish a mechanistic link between the 5-HT6 receptor, intracellular cAMP, and GIDs in transplanted PD patients. This effect is thought to be mediated through counteraction of the D2 autoreceptor feedback inhibition, resulting in a dysplastic DA release from the transplant.
“DREADD modulation of transplanted DA neurons reveals a novel serotonin dependent Parkinsonian dyskinesia mechanism mediated by the 5-HT6 receptor” by Patrick Aldrin-Kirk, Andreas Heuer, Gang Wang, Bengt Mattsson, Martin Lundblad, Malin Parmar, and Tomas Björklund in Neuron. Published online May 5 2016 doi:10.1016/j.neuron.2016.04.017






