Summary: A new synthetic conduit can bridge large nerve gaps by guiding the regrowth of neurons. When implanted into the arms of macaques with nerve defects in their arms, the conduit boosted neurogenesis and the nerve’s ability to conduct signals for a year.
Source: AAAS
A team of scientists has created a biodegradable, synthetic conduit that repairs large gaps in injured nerves, which supported recovery and accelerated neuronal healing in a macaque model.
The synthetic nerve conduits could offer a viable alternative to autografts – the current gold standard treatment – for supporting the regeneration of nerves in patients who have experienced trauma and severe injuries.
Traumas or surgical procedures can damage the body’s peripheral nerves, resulting in gaps between the nerves that impair movement and daily life. Peripheral nerves do have the ability to slowly regenerate across small gaps with some assistance, but larger gaps from more severe injuries are more challenging to heal.
Clinicians treat large nerve gaps by transplanting nerve tissue from elsewhere in the body – called an autograft – but this approach doesn’t work for all types of injuries and can cause pain or a loss of sensation.
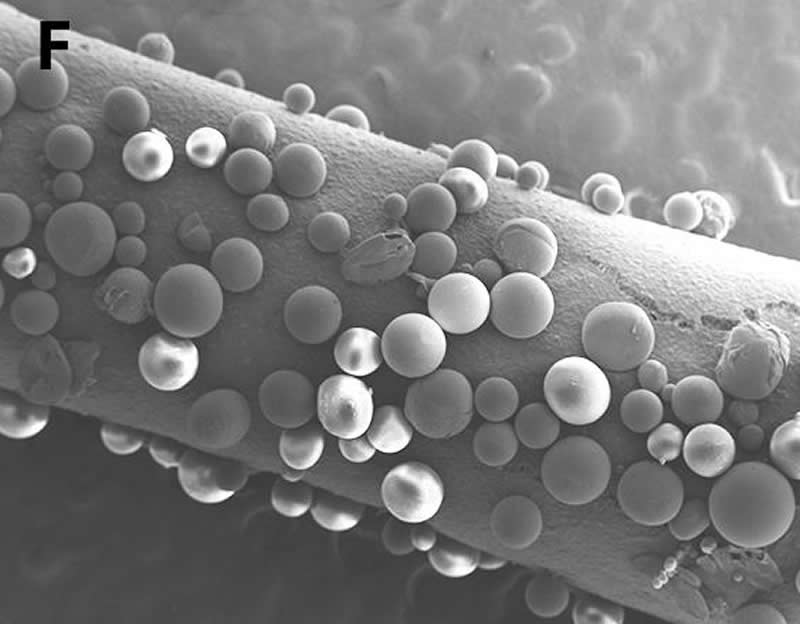
Building on previous work in rats, Neil Fadia and colleagues tested a synthetic conduit that can bridge large nerve gaps by guiding the regrowth of neurons. Their device is a small, tube-shaped object made of a biodegradable polyester with microspheres that release GDNF – a protein that supports the survival of neurons – embedded in the wall of the tube.
When implanted into macaques with large nerve defects in their arms, the nerve guide boosted nerve regeneration and the nerves’ ability to conduct signals over the course of a year.
The animals that received the conduits recovered their motor skills as well as those treated with autografts and showed superior recruitment of cells that sheathe neurons in myelin, an important protein that insulates nerves.
Source:
AAAS
Media Contacts:
Science Press Package Team – AAAS
Image Source:
The image is credited to N.B. Fadia et al., Science Translational Medicine (2019).
Original Research: Closed access
“Long-gap peripheral nerve repair through sustained release of a neurotrophic factor in nonhuman primates”. Neil B. Fadia, et al.
Science Translational Medicine doi:10.1126/scitranslmed.aav7753.
Abstract
Long-gap peripheral nerve repair through sustained release of a neurotrophic factor in nonhuman primates
Severe injuries to peripheral nerves are challenging to repair. Standard-of-care treatment for nerve gaps >2 to 3 centimeters is autografting; however, autografting can result in neuroma formation, loss of sensory function at the donor site, and increased operative time. To address the need for a synthetic nerve conduit to treat large nerve gaps, we investigated a biodegradable poly(caprolactone) (PCL) conduit with embedded double-walled polymeric microspheres encapsulating glial cell line–derived neurotrophic factor (GDNF) capable of providing a sustained release of GDNF for >50 days in a 5-centimeter nerve defect in a rhesus macaque model. The GDNF-eluting conduit (PCL/GDNF) was compared to a median nerve autograft and a PCL conduit containing empty microspheres (PCL/Empty). Functional testing demonstrated similar functional recovery between the PCL/GDNF-treated group (75.64 ± 10.28%) and the autograft-treated group (77.49 ± 19.28%); both groups were statistically improved compared to PCL/Empty-treated group (44.95 ± 26.94%). Nerve conduction velocity 1 year after surgery was increased in the PCL/GDNF-treated macaques (31.41 ± 15.34 meters/second) compared to autograft (25.45 ± 3.96 meters/second) and PCL/Empty (12.60 ± 3.89 meters/second) treatment. Histological analyses included assessment of Schwann cell presence, myelination of axons, nerve fiber density, and g-ratio. PCL/GDNF group exhibited a statistically greater average area occupied by individual Schwann cells at the distal nerve (11.60 ± 33.01 μm2) compared to autograft (4.62 ± 3.99 μm2) and PCL/Empty (4.52 ± 5.16 μm2) treatment groups. This study demonstrates the efficacious bridging of a long peripheral nerve gap in a nonhuman primate model using an acellular, biodegradable nerve conduit.






