Summary: Researchers identified a reduction in function in the lateral orbitofrontal cortex of obese mice.
Source: University of Calgary
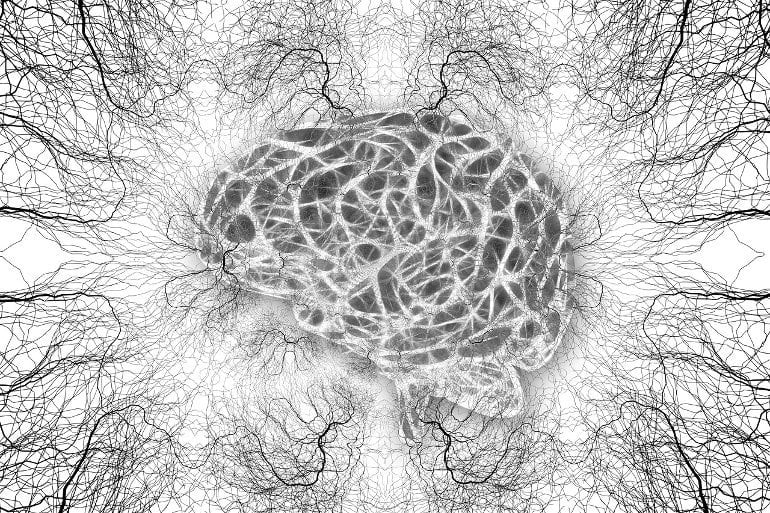
University of Calgary researchers find diet-induced obesity is linked to a functional change in the brain.
The study published in Nature Neuroscience finds that in obese mice there is a reduction in function of the brain’s brake signal located in the lateral orbitofrontal cortex. This region of the brain is involved in decision making about rewards and whether action should be taken to get rewards.
“We all change how we value food,” says Dr. Stephanie Borgland, PhD, professor at the Cumming School of Medicine and senior author on the study. “For example, when you’re hungry, a chocolate bar is a high value food. If you were forced to eat five or six chocolate bars though, you would become averse to it. This process is called devaluation.”
Researchers have long known that the brain is integral to controlling decisions about eating, but only now have they identified the specific part of the brain involved in devaluing food changes as obesity develops. Using mice, the Borgland lab adapted three devaluation methods commonly used to examine changes in goal-directed behaviour in obese mice.
“We discovered that if we essentially turned off the brake signal in the lateral orbitofrontal cortex, then our lean mice continued to work for sucrose even though they just consumed enough to be fully sated,” says Dr. Lauren Seabrook, PhD candidate and the lead investigator of this study, “When we restored normal activity in the orbitofrontal cortex of obese mice, mice regained the ability to devalue the sucrose and control over eating habits.”
Approximately one in four Canadian adults (26.6 percent) are currently living with obesity. Diet-induced obesity, along with metabolic disease, is a major health concern and is associated with multiple diseases including type 2 diabetes, stroke, cancer and depression.
“Our research is confirming that overeating has nothing to do with personal responsibility. It has to do with changes in the way the brain works in response to our food environment,” says Borgland.
“There is so much stigma with obesity. You would never hear anyone stigmatising someone with a brain change due to Multiple Sclerosis or Parkinson’s. Why are we doing it with obesity?”
The researchers are now conducting a pilot-study to explore the impact of this discovery on humans. If you are interested in learning more about the study you can email or leave a message at 403-210-6170.
Lauren Seabrook, PhD’22, and Lindsay Naef, PhD, contributed equally to the study.
About this obesity and neuroscience research news
Author: Kyle Marr
Source: University of Calgary
Contact: Kyle Marr – University of Calgary
Image: The image is in the public domain
Original Research: Closed access.
“Disinhibition of the orbitofrontal cortex biases decision-making in obesity” by Stephanie Borgland et al. Nature Neuroscience
Abstract
Disinhibition of the orbitofrontal cortex biases decision-making in obesity
The lateral orbitofrontal cortex (lOFC) receives sensory information about food and integrates these signals with expected outcomes to guide future actions, and thus may play a key role in a distributed network of neural circuits that regulate feeding behavior.
Here, we reveal a new role for the lOFC in the cognitive control of behavior in obesity. Food-seeking behavior is biased in obesity such that in male obese mice, behaviors are less flexible to changes in the perceived value of the outcome.
Obesity is associated with reduced lOFC inhibitory drive and chemogenetic reduction in GABAergic neurotransmission in the lOFC induces obesity-like impairments in goal-directed behavior. Conversely, pharmacological or optogenetic restoration of inhibitory neurotransmission in the lOFC of obese mice reinstates flexible behavior.
Our results indicate that obesity-induced disinhibition of the lOFC leads to a failure to update changes in the value of food with satiety, which in turn may influence how individuals make decisions in an obesogenic environment.







