Summary: Switching to a Mediterranean diet significantly improved symptoms of depression in young men, a new study reports.
Source: University of Sydney
Young men with a poor diet saw a significant improvement in their symptoms of depression when they switched to a healthy Mediterranean diet, a new study shows.
Depression is a common mental health condition that affects approximately 1 million Australians each year. It is a significant risk factor for suicide, the leading cause of death in young adults.
The 12-week randomized control trial, conducted by researchers from the University of Technology Sydney, was recently published in the peer-reviewed American Journal of Clinical Nutrition.
Lead researcher Jessica Bayes, a PhD candidate in the UTS Faculty of Health, said the study was the first randomized clinical trial to assess the impact of a Mediterranean diet on the symptoms of depression in young men (aged 18-25).
“We were surprised by how willing the young men were to take on a new diet,” Bayes said. “Those assigned to the Mediterranean diet were able to significantly change their original diets, under the guidance of a nutritionist, over a short time frame.”
“It suggests that medical doctors and psychologists should consider referring depressed young men to a nutritionist or dietitian as an important component of treating clinical depression,” she said.
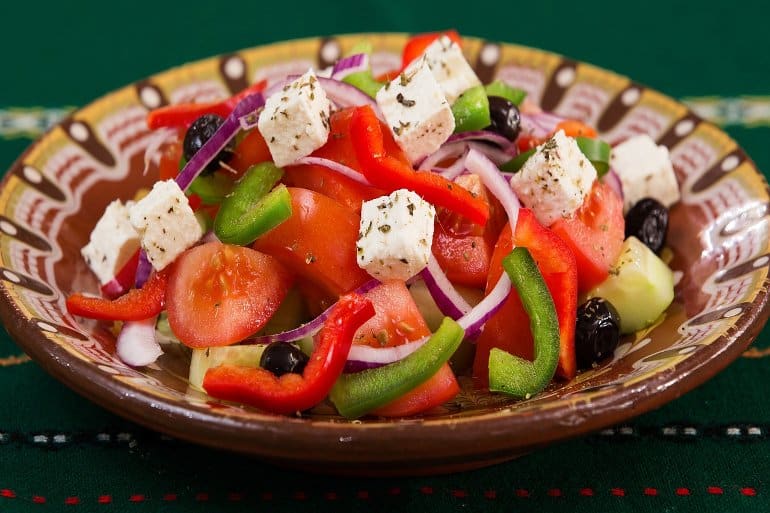
The study contributes to the emerging field of nutritional psychiatry, which aims to explore the effect that specific nutrients, foods and dietary patterns can have on mental health. The diet used in the study was rich in colorful vegetables, legumes and wholegrains, oily fish, olive oil, and raw, unsalted nuts.
“The primary focus was on increasing diet quality with fresh wholefoods while reducing the intake of ‘fast’ foods, sugar and processed red meat,” Bayes said.
“There are lots of reasons why scientifically we think food affects mood. For example, around 90 per cent of serotonin, a chemical that helps us feel happy, is made in our gut by our gut microbes. There is emerging evidence that these microbes can communicate to the brain via the vagus nerve, in what is called the gut-brain axis.
“To have beneficial microbes, we need to feed them fibre, which is found in legumes, fruits and vegetables,” she said.
Roughly 30 percent of depressed patients fail to adequately respond to standard treatments for major depressive disorder such as cognitive behaviour therapy and anti-depressant medications.
“Nearly all our participants stayed with the program, and many were keen to continue the diet once the study ended, which shows how effective, tolerable and worthwhile they found the intervention.”
About this diet and depression research news
Author: Leilah Schubert
Source: University of Sydney
Contact: Leilah Schubert – University of Sydney
Image: The image is in the public domain
Original Research: Closed access.
“The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND” study): A Randomized Control Trial” by Jessica Bayes et al. American Journal of Clinical Nutrition
Abstract
The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND” study): A Randomized Control Trial
Background
Depression is a common mental health condition which affects 1 in 8 males each year, especially young adults. Young adulthood offers an opportunity for early dietary interventions, with research suggesting that a Mediterranean diet (MD) could be beneficial in treating depression.
Objective
This study aimed to determine if a MD can improve depressive symptoms in young males with clinical depression.
Methods
A 12-week, parallel-group, open-label, randomized control trial was conducted to assess the effect of a MD intervention in the treatment of moderate to severe depression in young males (18-25 years). Befriending therapy was chosen for the control group. Assessments were taken at baseline, week 6 and week 12. MD adherence was measured with the Mediterranean Adherence Score (MEDAS). The primary outcome measure was the Beck Depression Inventory Scale (BDI-II) and secondary outcome was Quality of Life (QoL).
Results
A total of 72 participants completed the study. After 12 weeks, the MEDAS scores were significantly higher in the MD group compared to the befriending group (Mean diff: 7.8, 95% CI: 7.23, 8.37, p<0.001). The mean change in BDI-II score was significantly higher in the MD group compared to the befriending group at week 12 (Mean diff: 14.4, 95% CI: 11.41, 17.39, p<0.001). The mean change in QoL score was also significantly higher in the MD group compared to the befriending group at week 12 (Mean diff: 12.7, 95% CI: 7.92, 17.48), p<0.001).
Conclusion
Our results demonstrate that compared to befriending, a MD intervention leads to significant increases in MEDAS score, decreases in BDI-II score and increases in QoL scores. These results highlight the important role of nutrition for the treatment of depression and should inform advice given by clinicians to this specific demographic population.






