Summary: Researchers have identified genetic variations in brain cells, particularly microglia and oligodendrocytes, that influence both aging and Alzheimer’s risk. These variations impact how cells function as they age, potentially priming some individuals for dementia.
The findings suggest two sequential processes: genetic factors influence aging, which may predispose individuals to Alzheimer’s. Human-specific genetic links to Alzheimer’s highlight the unique vulnerability of human brain cells to the disease.
Key Facts
- Brain Cell Role: Microglia and oligodendrocytes show genetic variations tied to ageing and Alzheimer’s risk.
- Sequential Processes: Ageing-related gene variants may predispose individuals to dementia, affecting when and how Alzheimer’s develops.
- Human-Specific Findings: Genetic links to Alzheimer’s were observed only in humans, highlighting unique susceptibilities in human brain cells.
Source: UCL
Genetic differences that contribute to how long a person will live and their risk of Alzheimer’s disease have been identified by researchers at UCL and the UK Dementia Research Institute (UK DRI).
The study, published in Brain, found that genetic variations in brain cells, particularly the immune cells in the brain (microglia) and the cells that support nerve cells (oligodendrocytes), are linked to both ageing and Alzheimer’s.
The researchers hope that the findings will highlight potential new targets for treating Alzheimer’s and provide a deeper understanding of how our brains age.
Senior author, Dr Dervis Salih (UCL Queen Square Institute of Neurology and UK Dementia Research Institute at UCL), said: “Our research highlights how genetic variation in certain brain cells can provide new opportunities for drug discovery of novel molecular targets for treatment.
“By understanding how these cells change with age and their role in Alzheimer’s, we gain a deeper insight into the ageing brain, offering hope for innovative and preventative therapies and a brighter future for families affected by this life-changing disease.”
To understand the genetic factors behind ageing and Alzheimer’s, the team used large datasets of genetic information from people with Alzheimer’s (21,982 people) and those without (41,944 people) from the International Genomics of Alzheimer’s Projects (IGAP), alongside European ancestry data on ageing – including the length of time a person was healthy (300,477 people), their longevity (11,262 people), and the lifespan of their parents (1,012,240 parents from a study from the University of Edinburgh).
The team then analysed these datasets to find the significance of certain genes with relation to both ageing and Alzheimer’s.
They also used RNA sequencing data – a technique used to help understand which genes are active and how much they change with ageing and disease – from both mice and people to study gene activity (how cells function and respond to their environment).
The researchers found that genetic differences linked to Alzheimer’s are common in microglia and oligodendrocytes, as both change with age and are linked to Alzheimer’s risk.
These changes were observed in both humans and mice. However, only humans showed significant genetic links to Alzheimer’s, suggesting that aging in human brain cells might make them more susceptible to dementia.
Researchers found that certain genetic variants were linked to how cells respond to aging, while others were linked to dementia.
A few gene variants were associated with both aging and dementia, including APOE (a gene that provides instructions for making a protein called apolipoprotein E, which helps transport fats and cholesterol in the bloodstream), which had a strong effect.
This data indicates two sequential processes: aging and then dementia. This suggests that aging gene variants may prime some people for dementia, influencing when and how Alzheimer’s develops.
It may also explain why some people develop dementia when they reach 70-80 years of age, and why some people are still mentally sharp when they are much older.
Dr. Salih said: “Genetic differences in microglia and oligodendrocytes affect how the cells function during aging, either in a healthy way or an activated way related to the disease.
“By understanding these key genes, we might be able to develop new tests and biomarkers that will help slow brain aging and the progression of Alzheimer’s Disease.”
This work was performed in collaboration with Professor Valentina Escott-Price (UK Dementia Research Institute at Cardiff University) and Professor Sir John Hardy (UCL Queen Square Institute of Neurology and UK Dementia Research Institute at UCL).
The study was funded by the UK DRI and Dr Salih is also by funded by Alzheimer’s Research UK and the Medical Research Council NMGN Ageing Cluster.
Professor Escott-Price said: “These results have been and can only be achieved by combining large scale human, animal and molecular data, and sharing expertise across disciplines including biology, mathematics and informatics.”
About this genetics, aging, and Alzheimer’s disease research news
Author: Poppy Tombs
Source: UCL
Contact: Poppy Tombs – UCL
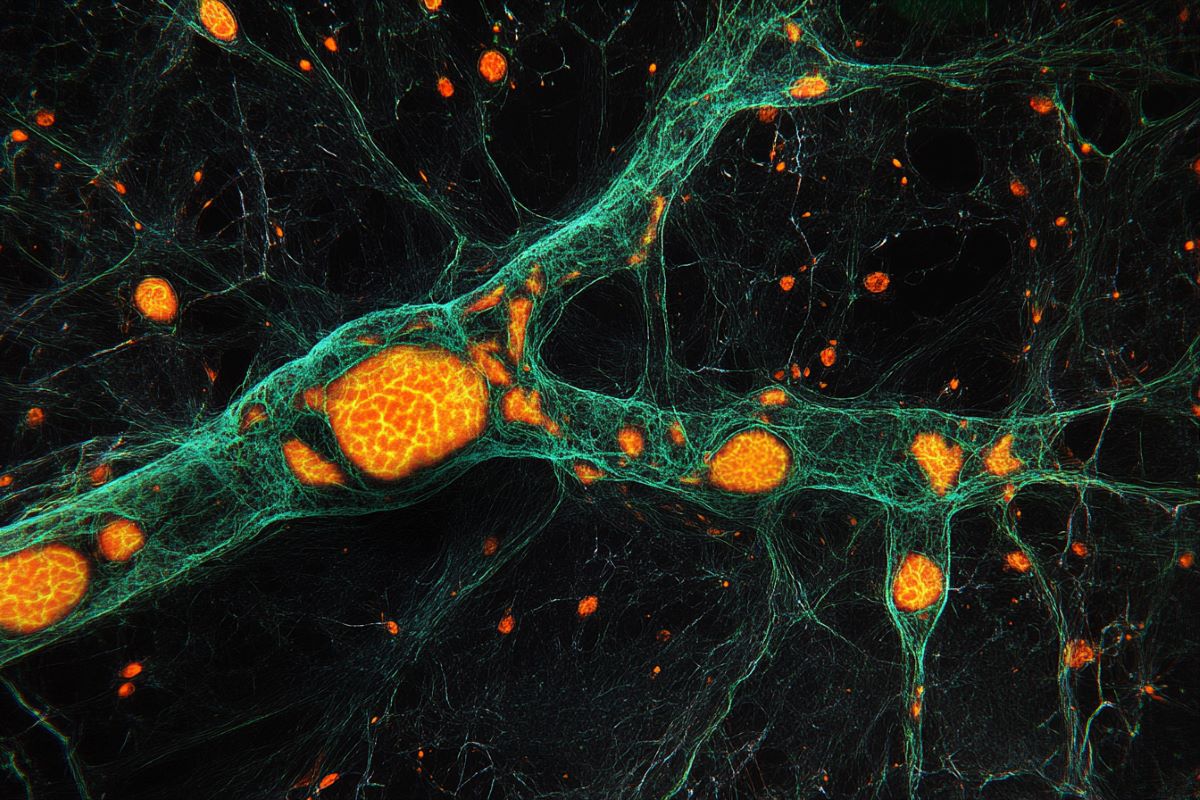
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Human longevity and Alzheimer’s disease variants act via microglia and oligodendrocyte gene networks” by Dervis Salih et al. Brain
Abstract
Human longevity and Alzheimer’s disease variants act via microglia and oligodendrocyte gene networks
Ageing underlies functional decline of the brain and is the primary risk factor for several neurodegenerative conditions, including Alzheimer’s disease (AD). However, the molecular mechanisms that cause functional decline of the brain during ageing, and how these contribute to AD pathogenesis, are not well understood.
The objective of this study was to identify biological processes that are altered during ageing in the hippocampus and that modify Ad risk and lifespan, and then to identify putative gene drivers of these programmes.
We integrated common human genetic variation associated with human lifespan or Ad from genome-wide association studies with co-expression transcriptome networks altered with age in the mouse and human hippocampus.
Our work confirmed that genetic variation associated with Ad was enriched in gene networks expressed by microglia responding to ageing and revealed that they were also enriched in an oligodendrocytic gene network.
Compellingly, longevity-associated genetic variation was enriched in a gene network expressed by homeostatic microglia whose expression declined with age.
The genes driving this enrichment include CASP8 and STAT3, highlighting a potential role for these longevity-associated genes in the homeostatic functions of innate immune cells, and these genes might drive ‘inflammageing’.
Thus, we observed that gene variants contributing to ageing and AD balance different aspects of microglial and oligodendrocytic function. Furthermore, we also highlight putative Ad risk genes, such as LAPTM5, ITGAM and LILRB4, whose association with Ad falls below genome-wide significance but show strong co-expression with known Ad risk genes in these networks.
Indeed, five of the putative risk genes highlighted by our analysis, ANKH, GRN, PLEKHA1, SNX1 and UNC5CL, have subsequently been identified as genome-wide significant risk genes in a subsequent genome-wide association study with larger sample size, validating our analysis.
This work identifies new genes that influence ageing and AD pathogenesis, and highlights the importance of microglia and oligodendrocytes in the resilience of the brain against ageing and AD pathogenesis.
Our findings have implications for developing markers indicating the physiological age of the brain and new targets for therapeutic intervention.







