Summary: Temozolomide, a chemotherapy drug used to treat brain cancer, could increase risks of developing depression by preventing neurogenesis, a new study reports.
Source: King’s College London.
A chemotherapy drug used to treat brain cancer may increase vulnerability to depression by stopping new brain cells from growing, according to a new King’s College London study out today in Translational Psychiatry.
Depression is thought to be the least recognised symptom in people with cancer. It has previously been difficult to determine if some people with cancer develop depression as a result of chemotherapy or the stress of having cancer itself.
Although an early animal study, these findings are the first to suggest that chemotherapy causes behavioural and biological brain changes related to depression that are separate from the psychological distress resulting from a cancer diagnosis.
Recent research has shown that depression is most common in cancer patients who have brain cancer. Studies show that around 30 per cent of patients with brain cancer experience depression and the disorder is thought to be highly under-diagnosed. For example, one recent study pointed out that 90 per cent of patients self-reported symptoms of depression, whereas only 20 per cent were classified as having clinical depression.
Most cancer patients are treated with chemotherapy as a lifesaving intervention that stops all cells in the body from dividing. The primary outcome of this treatment is to kill rapidly dividing cancer cells, but disrupting this process can have potential side effects related to cell division, such as hair loss. Researchers now know from animal studies that chemotherapy may similarly stop the growth of new brain cells (neurogenesis).
In their new study, scientists from King’s College London set out to examine whether the effects of chemotherapy on neurogenesis could alter biological brain mechanisms which increase vulnerability for depression.
They administered a chemotherapy drug to mice called Temozolomide (TMZ), using the same procedure that human patients would experience in a clinic. Mice receiving the chemotherapy drug showed a significant reduction in growth of new brain cells in the hippocampus – a region associated with emotion and memory. Results from the study show that the more the drug decreased neurogenesis, the greater the increase in stress hormones when exposed to stress.
When researchers looked at the mice’s behaviour following treatment, they observed several changes related to depression, including robust deficits in novelty processing and a decrease in preference for a rewarding sugar solution. A lack of pleasure seeking, as observed in mice that received the chemotherapy drug, is a core diagnostic symptom of depression.
Dr Martin Egeland, first author of the study, from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London, said: ‘Although these preliminary findings are based on mice, our results suggest that chemotherapy may stunt the growth of new brain cells, which has biological and behavioural consequences that may leave people less able to cope with the stress of having cancer.
‘Despite the potential side effects, chemotherapy is essential for increasing survival rates in cancer patients. However, understanding the specific effects of chemotherapy on mood could lead to improved treatments and increase quality of life for those affected by cancer.’

Dr Sandrine Thuret, senior author of the study also from the IoPPN at King’s College London, said: ‘Our study highlights the importance of protecting brain stem cells or building up a reserve of cells before cancer treatment. This could help to preserve the mood and cognitive functions these cells are known to regulate, and could also improve quality of life for people with cancer.
‘We now need to explore whether neurogenesis enhancing interventions or drugs, such as antidepressants, can alleviate this deficit in new brain cells after chemotherapy takes place.’
Funding: This study was funded principally by an EU-FP7 Marie Curie fellowship.
Source: Jack Stonebridge – King’s College London
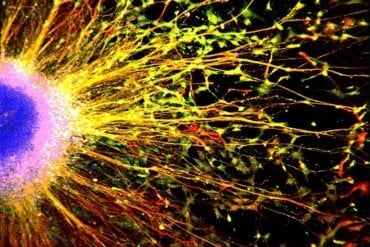
Image Source: NeuroscienceNews.com image is in the public domain and is credited to the National Cancer Institute.
Original Research: Full open access research for “Depletion of adult neurogenesis using the chemotherapy drug temozolomide in mice induces behavioural and biological changes relevant to depression” by M Egeland, C Guinaudie, A Du Preez, K Musaelyan, P A Zunszain, C Fernandes, C M Pariante & S Thuret in Translational Psychiatry. Published online April 25 2017 doi:10.1038/tp.2017.68
[cbtabs][cbtab title=”MLA”]King’s College London “Chemo Drug May Increase Vulnerability to Depression.” NeuroscienceNews. NeuroscienceNews, 25 April 2017.
<https://neurosciencenews.com/depression-chemotherapy-6497/>.[/cbtab][cbtab title=”APA”]King’s College London (2017, April 25). Chemo Drug May Increase Vulnerability to Depressione. NeuroscienceNew. Retrieved April 25, 2017 from https://neurosciencenews.com/depression-chemotherapy-6497/[/cbtab][cbtab title=”Chicago”]King’s College London “Chemo Drug May Increase Vulnerability to Depression.” https://neurosciencenews.com/depression-chemotherapy-6497/ (accessed April 25, 2017).[/cbtab][/cbtabs]
Abstract
Depletion of adult neurogenesis using the chemotherapy drug temozolomide in mice induces behavioural and biological changes relevant to depression
Numerous studies have examined links between postnatal neurogenesis and depression using a range of experimental methods to deplete neurogenesis. The antimitotic drug temozolomide (TMZ) has previously been used successfully as an experimental tool in animals to deplete adult neurogenesis and is used regularly on human patients as a standard chemotherapy for brain cancer. In this study, we wanted to evaluate whether TMZ as a model for chemotherapy treatment could affect parameters related to depression in an animal model. Prevalence rates of depression in patients is thought to be highly underdiagnosed, with some studies reporting rates as high as 90%. Results from this study in mice, treated with a regimen of TMZ similar to humans, exhibited behavioural and biochemical changes that have relevance to the development of depression. In particular, behavioural results demonstrated robust deficits in processing novelty and a significant increase in the corticosterone response. Quantification of neurogenesis using a novel sectioning method, which clearly evaluates dorsal and ventral neurogenesis separately, showed a significant correlation between the level of ventral neurogenesis and the corticosterone response. Depression is a complex disorder with discoveries regarding its neurobiology and how it relates to behaviour being only in their infancy. The findings presented in this study demonstrate that chemotherapy-induced decreases in neurogenesis results in previously unreported behavioural and biochemical consequences. These results, we argue, are indicative of a biological mechanism, which may contribute to the development of depression in patients being treated with chemotherapy and is separate from the mental distress resulting from a cancer diagnosis.
“Depletion of adult neurogenesis using the chemotherapy drug temozolomide in mice induces behavioural and biological changes relevant to depression” by M Egeland, C Guinaudie, A Du Preez, K Musaelyan, P A Zunszain, C Fernandes, C M Pariante & S Thuret in Translational Psychiatry. Published online April 25 2017 doi:10.1038/tp.2017.68