Summary: Iron accumulation in the brain’s neocortex has been linked to cognitive decline in people with Alzheimer’s disease.
Source: RSNA
Researchers using MRI have found that iron accumulation in the outer layer of the brain is associated with cognitive deterioration in people with Alzheimer’s disease, according to a study published in the journal Radiology.
Alzheimer’s disease is a progressive type of dementia that impairs and eventually destroys memory and other brain functions. There is no cure, although some treatments are thought to slow the progression.
Previous research has linked abnormally high levels of iron in the brain with Alzheimer’s disease. Iron deposition correlates with amyloid beta, a protein that clumps together in the brains of people with Alzheimer’s disease to form plaques that collect between neurons and disrupt cell function. Associations have also been found between iron and neurofibrillary tangles, abnormal accumulations of a protein called tau that collect inside neurons. These tangles block the neuron’s transport system, which harms the communication between neurons.
It is known that deep gray matter structures of patients with Alzheimer’s disease contain higher brain iron concentrations. Less is known about the neocortex, the deeply grooved outer layer of the brain that is involved with language, conscious thought and other important functions. The neocortex is challenging to assess by MRI, as the anatomy of the area makes MRI prone to distortions, signal decays and artifacts.
“The best solution to minimize these artifacts would be using ultra-high-resolution scans,” said study coauthor Reinhold Schmidt, M.D., professor of neurology and chairman of the Department of Neurology at the Medical University of Graz in Graz, Austria. “However, in the clinical setting, scan time is a limiting factor, and a compromise has to be found.”
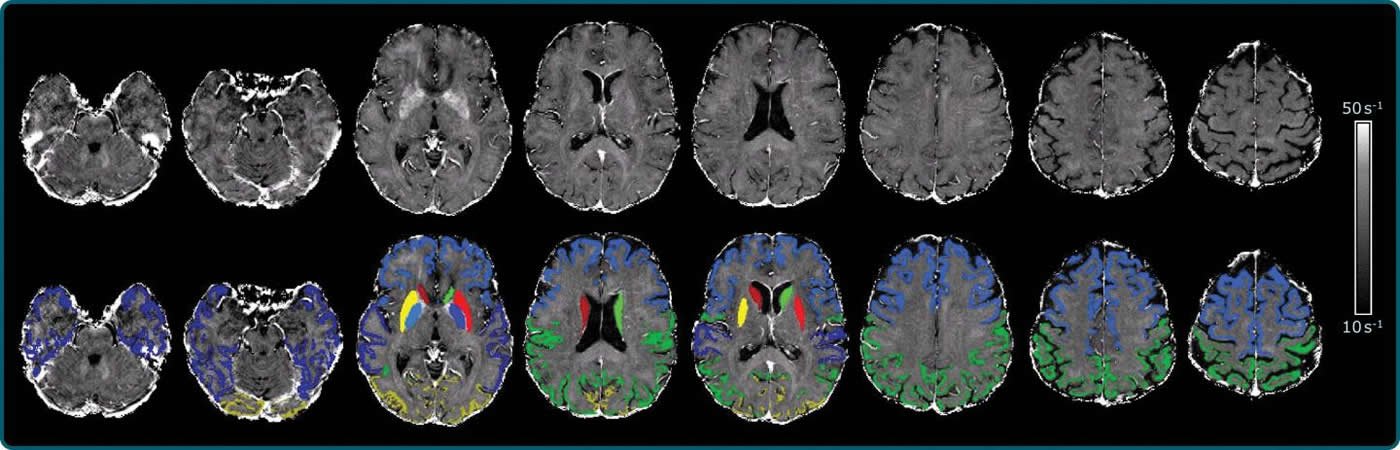
For the new study, Dr. Schmidt and colleagues developed an approach using a 3T MRI scanner that allowed the best tradeoff between resolution and scan time, along with postprocessing to correct the influence of the distortions.
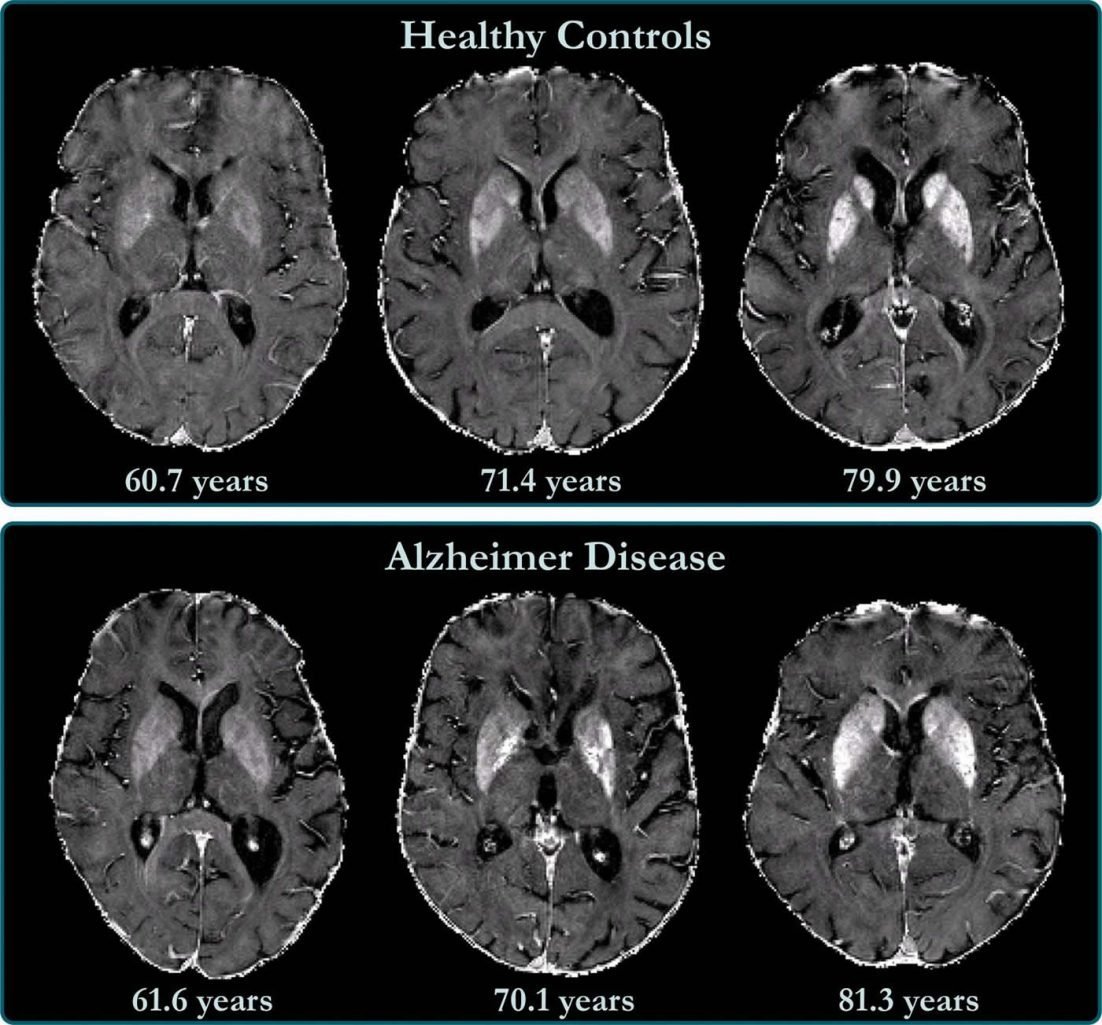
They used the MRI system to investigate baseline levels of brain iron in 100 individuals with Alzheimer’s disease and 100 healthy controls. Of the 100 participants with Alzheimer’s disease, 56 had subsequent neuropsychological testing and brain MRI at a mean follow-up of 17 months.
The technique enabled the researchers to create a map of brain iron, determining iron levels in parts of the brain like the temporal lobes, or the areas of the brain lying underneath the temples, and the occipital lobes in the back of the head.
“We found indications of higher iron deposition in the deep gray matter and total neocortex, and regionally in temporal and occipital lobes, in Alzheimer’s disease patients compared with age-matched healthy individuals,” Dr. Schmidt said.
The brain iron accumulation was associated with cognitive deterioration independently of brain volume loss. Changes in iron levels over time in the temporal lobes correlated with cognitive decline in individuals with Alzheimer’s disease.
“These results are all in keeping with the view that high concentrations of iron significantly promote amyloid beta deposition and neurotoxicity in Alzheimer’s disease,” Dr. Schmidt said.
The results point to a potential role in Alzheimer’s disease treatment for drugs that reduce the iron burden in the brain. These drugs, known as chelators, can remove excess iron from the body.
“Our study provides support for the hypothesis of impaired iron homeostasis in Alzheimer’s disease and indicates that the use of iron chelators in clinical trials might be a promising treatment target,” Dr. Schmidt said. “MRI-based iron mapping could be used as a biomarker for Alzheimer’s disease prediction and as a tool to monitor treatment response in therapeutic studies.”
About this neuroscience research article
Source:
RSNA
Media Contacts:
Linda Brooks – RSNA
Image Source:
The images are credited to RSNA.
Original Research: Open access
“Cross-sectional and Longitudinal Assessment of Brain Iron Level in Alzheimer Disease using 3-T MRI” by Anna Damulina, Lukas Pirpamer, Martin Soellradl, Maximilian Sackl, Christian Tinauer, Edith Hofer, Christian Enzinger, Benno Gesierich, Marco Duering, Stefan Ropele, Reinhold Schmidt, Christian Langkammer. Radiology
Abstract
Cross-sectional and Longitudinal Assessment of Brain Iron Level in Alzheimer Disease using 3-T MRI
Background
Deep gray matter structures in patients with Alzheimer disease (AD) contain higher brain iron concentrations. However, few studies have included neocortical areas, which are challenging to assess with MRI.
Purpose
To investigate baseline and change in brain iron levels using MRI at 3 T with R2* relaxation rate mapping in individuals with AD compared with healthy control (HC) participants.
Materials and Methods
In this prospective study, participants with AD recruited between 2010 and 2016 and age-matched HC participants selected from 2010 to 2014 were evaluated. Of 100 participants with AD, 56 underwent subsequent neuropsychological testing and brain MRI at a mean follow-up of 17 months. All participants underwent 3-T MRI, including R2* mapping corrected for macroscopic B0 field inhomogeneities. Anatomic structures were segmented, and median R2* values were calculated in the neocortex and cortical lobes, basal ganglia (BG), hippocampi, and thalami. Multivariable linear regression analysis was applied to study the difference in R2* levels between groups and the association between longitudinal changes in R2* values and cognition in the AD group.
Results
A total of 100 participants with AD (mean age, 73 years ± 9 [standard deviation]; 58 women) and 100 age-matched HC participants (mean age, 73 years ± 9; 60 women) were evaluated. Median R2* levels were higher in the AD group than in the HC group in the BG (HC, 29.0 sec−1; AD, 30.2 sec−1; P = .01) and total neocortex (HC, 17.0 sec−1; AD, 17.4 sec−1; P < .001) and regionally in the occipital (HC, 19.6 sec−1; AD, 20.2 sec−1; P = .007) and temporal (HC, 16.4 sec−1; AD, 18.1 sec−1; P < .001) lobes. R2* values in the temporal lobe were associated with longitudinal changes in Consortium to Establish a Registry for Alzheimer’s Disease total score (β = −3.23 score/sec−1, P = .003) in participants with AD independent of longitudinal changes in brain volume.
Conclusion
Iron concentration in the deep gray matter and neocortical regions was higher in patients with Alzheimer disease than in healthy control participants. Change in iron levels over time in the temporal lobe was associated with cognitive decline in individuals with Alzheimer disease.







