Summary: Researchers report a clinical trial of a personalized vaccine that targets glioblastoma brain cancer has successfully improved survival rates for patients.
Source: WUSTL.
Most people with the deadly brain cancer glioblastoma die less than 18 months after diagnosis. But a multicenter clinical trial of a personalized vaccine that targets the aggressive cancer has indicated improved survival rates for such patients.
The study appears May 29 in the Journal of Translational Medicine.
The phase three clinical trial included 331 patients at over 80 sites in four countries. Among the trial participants was Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, which recruited one of the largest groups of patients in the trial. The patients were randomized to receive standard therapy plus the personalized vaccine, called DCVax-L, or standard therapy plus a placebo. Personalized vaccines are specifically tailored to individual patients.
According to the trial design, the vaccine group had twice the number of patients as the placebo group. Further, any patient in the trial was allowed to receive the vaccine if his or her cancer recurred or progressed after initial treatment. As such, almost 90 percent of all participants received the investigational vaccine.
The trial, which was funded by the vaccine maker, Northwest Biotherapeutics Inc., is ongoing to allow for continued study of patients who are living beyond what is expected of those diagnosed with glioblastoma.
As of the analysis detailed in the study, all 331 patients in the trial (including those who did and did not receive the vaccine) had a median survival of just over 23 months. One-hundred patients had an average overall survival of 40.5 months — more than three years — and were designated as “extended survivors.” Investigators are particularly interested in the latter group’s response to the vaccine, though they don’t yet know whether everyone in this group received the vaccine since the trial is ongoing and remains blinded. The continued blinding means neither the patients nor physicians know which patients are receiving the vaccine. But since the researchers reported that almost 90 percent of all participants received the vaccine at some point, the chances that the extended survivors are getting the vaccine, rather than placebo, are high.
“The overall patient population in the trial appears to live longer than we would typically see with current standard of care, and 30 percent of the patients have lived much longer than we would expect, given the typical course of this cancer,” said oncologist Jian L. Campian, MD, PhD, one of the study’s authors and a Washington University assistant professor of medicine who treats patients at Siteman Cancer Center. “In general, patients with this cancer live 15 to 17 months. The surprising part was that the 100 ‘extended survivors’ don’t appear to have the usual characteristics associated with a good prognosis. We are continuing to study these patients to understand why they have done so well.”
The personalized vaccine used was specific to each patient. After surgery to remove as much of the tumor as possible, a small amount of tumor tissue is processed and then exposed to the same patient’s own immune cells, called dendritic cells. Exposure to the tumor material essentially trains the dendritic cells to seek out and destroy tumor cells. These trained dendritic cells are returned to the patient as a vaccine injected in the arm. Relatively few vaccinations are needed: The first three are weeks apart; the next three are months apart; and then they continue with one vaccination every six months after the first year.
Campian said the vaccine had very few side effects, especially compared with standard treatment for this cancer, which includes surgery, radiation and chemotherapy. About 2 percent of participants (seven patients) experienced a serious adverse event — such as brain swelling or seizures — that may have been related to the vaccine, according to the researchers.
Source: WUSTL
Publisher: Organized by NeuroscienceNews.com.
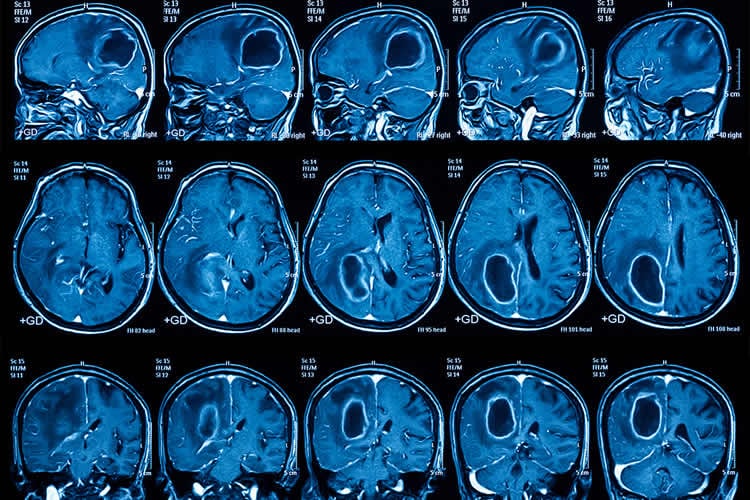
Image Source: NeuroscienceNews.com image is adapted from the WUSTL news release.
Original Research: Open access research for “First results on survival from a large Phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma” by Linda M. Liau , Keyoumars Ashkan, David D. Tran, Jian L. Campian, John E. Trusheim, Charles S. Cobbs, Jason A. Heth, Michael Salacz, Sarah Taylor, Stacy D. D’Andre, Fabio M. Iwamoto, Edward J. Dropcho, Yaron A. Moshel, Kevin A. Walter, Clement P. Pillainayagam, Robert Aiken, Rekha Chaudhary, Samuel A. Goldlust, Daniela A. Bota, Paul Duic, Jai Grewal, Heinrich Elinzano, Steven A. Toms, Kevin O. Lillehei, Tom Mikkelsen, Tobias Walpert, Steven R. Abram, Andrew J. Brenner, Steven Brem, Matthew G. Ewend, Simon Khagi, Jana Portnow, Lyndon J. Kim, William G. Loudon, Reid C. Thompson, David E. Avigan, Karen L. Fink, Francois J. Geoffroy, Scott Lindhorst, Jose Lutzky, Andrew E. Sloan, Gabriele Schackert, Dietmar Krex, Hans-Jorg Meisel, Julian Wu, Raphael P. Davis, Christopher Duma, Arnold B. Etame, David Mathieu, Santosh Kesari, David Piccioni, Manfred Westphal, David S. Baskin, Pamela Z. New, Michel Lacroix, Sven-Axel May, Timothy J. Pluard, Victor Tse, Richard M. Green, John L. Villano, Michael Pearlman, Kevin Petrecca, Michael Schulder, Lynne P. Taylor, Anthony E. Maida, Robert M. Prins, Timothy F. Cloughesy, Paul Mulholland and Marnix L. Bosch in Neural Networks. Published May 29 2018.
doi:10.1186/s12967-018-1507-6
[cbtabs][cbtab title=”MLA”]WUSTL “Brain Cancer Vaccine Effective in Some Patients.” NeuroscienceNews. NeuroscienceNews, 31 May 2018.
<https://neurosciencenews.com/brain-cancer-vaccine-9199/>.[/cbtab][cbtab title=”APA”]WUSTL (2018, May 31). Brain Cancer Vaccine Effective in Some Patients. NeuroscienceNews. Retrieved May 31, 2018 from https://neurosciencenews.com/brain-cancer-vaccine-9199/[/cbtab][cbtab title=”Chicago”]WUSTL “Brain Cancer Vaccine Effective in Some Patients.” https://neurosciencenews.com/brain-cancer-vaccine-9199/ (accessed May 31, 2018).[/cbtab][/cbtabs]
Abstract
First results on survival from a large Phase 3 clinical trial of an autologous dendritic cell vaccine in newly diagnosed glioblastoma
Background
Standard therapy for glioblastoma includes surgery, radiotherapy, and temozolomide. This Phase 3 trial evaluates the addition of an autologous tumor lysate-pulsed dendritic cell vaccine (DCVax®-L) to standard therapy for newly diagnosed glioblastoma.
Methods
After surgery and chemoradiotherapy, patients were randomized (2:1) to receive temozolomide plus DCVax-L (n = 232) or temozolomide and placebo (n = 99). Following recurrence, all patients were allowed to receive DCVax-L, without unblinding. The primary endpoint was progression free survival (PFS); the secondary endpoint was overall survival (OS).
Results
For the intent-to-treat (ITT) population (n = 331), median OS (mOS) was 23.1 months from surgery. Because of the cross-over trial design, nearly 90% of the ITT population received DCVax-L. For patients with methylated MGMT (n = 131), mOS was 34.7 months from surgery, with a 3-year survival of 46.4%. As of this analysis, 223 patients are ≥ 30 months past their surgery date; 67 of these (30.0%) have lived ≥ 30 months and have a Kaplan-Meier (KM)-derived mOS of 46.5 months. 182 patients are ≥ 36 months past surgery; 44 of these (24.2%) have lived ≥ 36 months and have a KM-derived mOS of 88.2 months. A population of extended survivors (n = 100) with mOS of 40.5 months, not explained by known prognostic factors, will be analyzed further. Only 2.1% of ITT patients (n = 7) had a grade 3 or 4 adverse event that was deemed at least possibly related to the vaccine. Overall adverse events with DCVax were comparable to standard therapy alone.
Conclusions
Addition of DCVax-L to standard therapy is feasible and safe in glioblastoma patients, and may extend survival.






