Summary: Researchers have succeeded in wirelessly recording both deep and surface human brain activity for an extended period of time while the patient was in their home environment.
Source: NIH
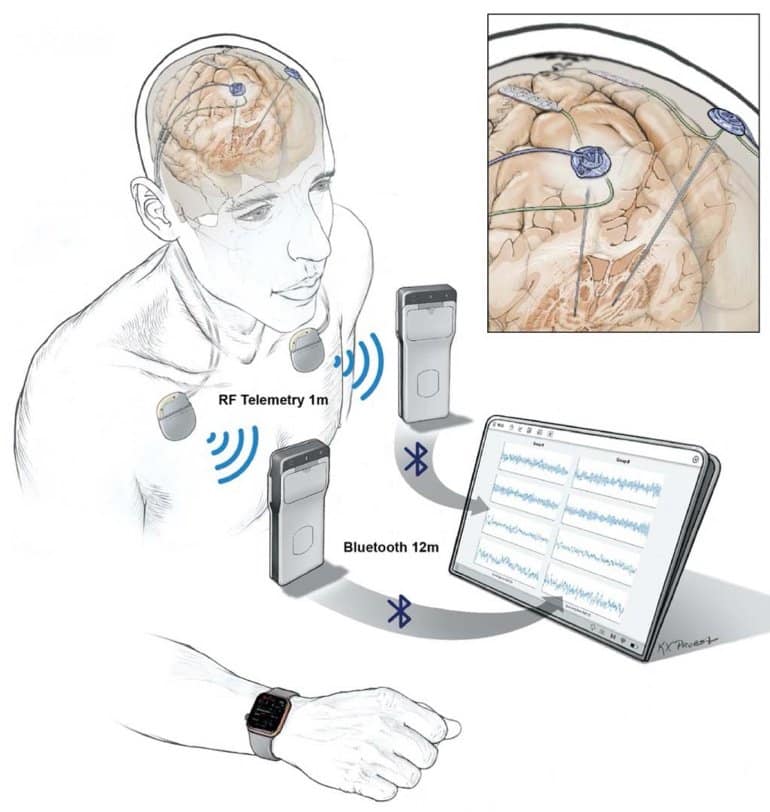
Researchers are now able to wirelessly record the directly measured brain activity of patients living with Parkinson’s disease and to then use that information to adjust the stimulation delivered by an implanted device. Direct recording of deep and surface brain activity offers a unique look into the underlying causes of many brain disorders; however, technological challenges up to this point have limited direct human brain recordings to relatively short periods of time in controlled clinical settings.
This project, published in the journal Nature Biotechnology, was funded by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies (BRAIN) Initiative.
“This is really the first example of wirelessly recording deep and surface human brain activity for an extended period of time in the participants’ home environment,” said Kari Ashmont, Ph.D., project manager for the NIH BRAIN Initiative. “It is also the first demonstration of adaptive deep brain stimulation at home.”
Deep brain stimulation (DBS) devices are approved by the U. S. Food and Drug Administration for the management of Parkinson’s disease symptoms by implanting a thin wire, or electrode, that sends electrical signals into the brain.
In 2018, the laboratory of Philip Starr, M.D., Ph.D. at the University of California, San Francisco, developed an adaptive version of DBS that adapts its stimulation only when needed based on recorded brain activity. In this study, Dr. Starr and his colleagues made several additional improvements to the implanted technology.
“This is the first device that allows for continuous and direct wireless recording of the entire brain signal over many hours,” said Dr. Starr. “That means we are able to perform whole brain recording over a long period of time while people are going about their daily lives.”
The implications of this type of recording are significant. The brain activity patterns (neural signatures) normally used to identify problems such as Parkinson’s disease symptoms have traditionally been recorded in clinical settings over short periods of time. This new technology makes it possible to validate those signatures during ordinary daily activities.
“If you ever hope to use in-hospital recordings to modify a disease state through adaptive stimulation, you must show that they are also valid in the real world,” said Dr. Starr.
Another advantage to recording over long periods of time is that distinct changes in brain activity (biomarkers) that could predict movement disorders can now be identified for individual patients. Ro’ee Gilron, Ph.D., a postdoctoral scholar in Dr. Starr’s lab and first author of this study, explained that this allows for a level of customized DBS treatment that was impossible to achieve previously.
“Because we are able to build a biomarker library for each patient, we can now program each DBS unit according to a patient’s individual needs,” said Dr. Gilron. “This includes personalized stimulation programs that adapt as the patient’s needs change throughout the day.”
One important consideration that arises is the ethical implication of (nearly) all-day brain recording. Since its beginning, the NIH BRAIN Initiative has recognized the importance of addressing potential ethical considerations pertaining to the development and use of devices that record or modulate brain activity.
For instance, the NIH BRAIN Neuroethics Working Group is a group of experts in neuroethics and neuroscience that serves to provide the NIH BRAIN Initiative with input relating to neuroethics–a field that studies the ethical, legal, and societal implications of neuroscience.
Alongside funding for neurotechnology research, the Initiative also funds research on the ethical implications of advancements in neurotechnology.
“We have had patients approach us with concerns regarding privacy,” said Dr. Starr. “Although we are not at the point where we can distinguish specific normal behaviors from brain activity recording, it is an absolutely legitimate concern. We have told patients to feel free to remove their wearable devices and to turn off their brain recordings whenever they engage in activities they would like to keep private.”
The patients were also invited to participate in NIH BRAIN Initiative-funded neuroethics projects looking to identify concerns about this new technology (MH114860). In addition, individuals who opted out of the implant project were interviewed about their decision. As recommended by a recent BRAIN 2.0 neuroethics report, this information will be used to develop ethical guidelines and protocols for future projects to achieve a healthy balance between discovery and privacy.
One unforeseen benefit of this study was that, because it required little to no direct contact with clinicians following surgery, it was ideally suited for the social distancing that is crucial during the COVID-19 pandemic. The technologies used for remote patient monitoring and telehealth were originally designed for the convenience of study subjects, but they have broader applications to other research projects that have been stalled due to COVID-19.
“The technologies we developed and used to communicate and work remotely with our patients can also allow those who do not live close to a clinic to receive ‘over the air’ updates for their devices and telehealth visits from their neurologists as they manage increasingly complex DBS devices,” said Dr. Gilron.
The importance of studying behavior in a natural environment such as the home as it relates to neural activity was emphasized in a recent BRAIN 2.0 neuroscience report. Dr. Ashmont stressed that this study is a significant step in that direction and is going to help scientists understand not only disorders but also the neural representation of behaviors in general.
Funding: This research was funded by a grant from the NIH BRAIN Initiative (NS100544).
About this neurotech research news
Source: NIH
Contact: Carl P. Wonders – NIH
Image: The image is credited to Starr lab, UCSF
Original Research: Closed access.
“Long-term wireless streaming of neural recordings for circuit discovery and adaptive stimulation in individuals with Parkinson’s disease” by Ro’ee Gilron, Simon Little, Randy Perrone, Robert Wilt, Coralie de Hemptinne, Maria S. Yaroshinsky, Caroline A. Racine, Sarah S. Wang, Jill L. Ostrem, Paul S. Larson, Doris D. Wang, Nick B. Galifianakis, Ian O. Bledsoe, Marta San Luciano, Heather E. Dawes, Gregory A. Worrell, Vaclav Kremen, David A. Borton, Timothy Denison & Philip A. Starr. Nature Biotechnology
Abstract
Long-term wireless streaming of neural recordings for circuit discovery and adaptive stimulation in individuals with Parkinson’s disease
Neural recordings using invasive devices in humans can elucidate the circuits underlying brain disorders, but have so far been limited to short recordings from externalized brain leads in a hospital setting or from implanted sensing devices that provide only intermittent, brief streaming of time series data.
Here, we report the use of an implantable two-way neural interface for wireless, multichannel streaming of field potentials in five individuals with Parkinson’s disease (PD) for up to 15 months after implantation. Bilateral four-channel motor cortex and basal ganglia field potentials streamed at home for over 2,600 h were paired with behavioral data from wearable monitors for the neural decoding of states of inadequate or excessive movement.
We validated individual-specific neurophysiological biomarkers during normal daily activities and used those patterns for adaptive deep brain stimulation (DBS).
This technological approach may be widely applicable to brain disorders treatable by invasive neuromodulation.







