Summary: Study finds amyloid-beta plaques may not be the cause of memory loss associated with Alzheimer’s disease, but instead a consequence of the disease. Regardless of the levels of amyloid plaques, researchers found individuals with high levels of amyloid peptide were cognitively normal. Higher levels of soluble amyloid beta peptide were also linked to people having a larger hippocampus.
Source: University of Cincinnati
Experts estimate more than 6 million Americans are living with Alzheimer’s dementia. But a recent study, led by the University of Cincinnati, sheds new light on the disease and a highly debated new drug therapy.
The UC-led study, conducted in collaboration with the Karolinska Institute in Sweden, claims that the treatment of Alzheimer’s disease might lie in normalizing the levels of a specific brain protein called amyloid-beta peptide. This protein is needed in its original, soluble form to keep the brain healthy, but sometimes it hardens into “brain stones” or clumps, called amyloid plaques.
The study, which appears in the journal EClinicalMedicine (published by the Lancet), comes on the heels of the FDA’s conditional approval of a new medicine, aducanumab, that treats the amyloid plaques.
“It’s not the plaques that are causing impaired cognition,” says Alberto Espay, the new study’s senior author and professor of neurology at UC. “Amyloid plaques are a consequence, not a cause,” of Alzheimer’s disease, says Espay, who is also a member of the UC Gardner Neuroscience Institute.
Alzheimer’s disease became widely known as “the long goodbye” in the late 20th century due to the disease’s slow deterioration of brain function and memory. It was over 100 years ago, however, that scientist Alois Alzheimer first identified plaques in the brain of patients suffering from the disease.
Since then, Espay says that scientists have focused on treatments to eliminate the plaques. But the UC team, he says, saw it differently: Cognitive impairment could be due to a decline in soluble amyloid-beta peptide instead of the corresponding accumulation of amyloid plaques.
To test their hypothesis, they analyzed the brain scans and spinal fluid from 600 individuals enrolled in the Alzheimer’s Disease Neuroimaging Initiative study, who all had amyloid plaques.
From there, they compared the amount of plaques and levels of the peptide in the individuals with normal cognition to those with cognitive impairment. They found that, regardless of the amount of plaques in the brain, the individuals with high levels of the peptide were cognitively normal.
They also found that higher levels of soluble amyloid-beta peptide were associated with a larger hippocampus, the area of the brain most important for memory.
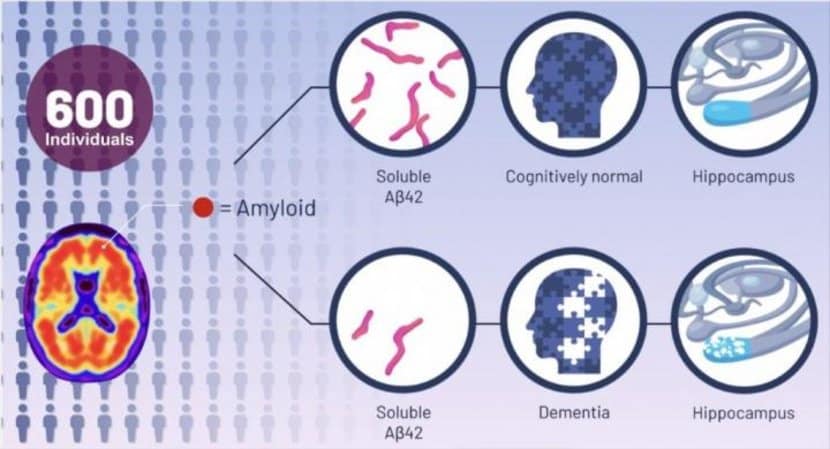
According to the authors, as we age most people develop amyloid plaques, but few people develop dementia. In fact, by the age of 85, 60% of people will have these plaques, but only 10% develop dementia, they say.
“The key discovery from our analysis is that Alzheimer’s disease symptoms seem dependent on the depletion of the normal protein, which is in a soluble state, instead of when it aggregates into plaques,” says co-author Kariem Ezzat from the Karolinska Institute.
The most relevant future therapeutic approach for the Alzheimer’s program will be replenishing these brain soluble proteins to their normal levels, says Espay.
The research team is now working to test their findings in animal models. If successful, future treatments may be very different from those tried over the last two decades. Treatment, says Espay, may consist of increasing the soluble version of the protein in a manner that keeps the brain healthy while preventing the protein from hardening into plaques.
Co-authors include: Andrea Sturchio, University of Cincinnati, and Samir EL Andaloussi, Karolinska Institute.
Funding: The research was funded by the UC Gardner Neuroscience Institute.
The authors disclose that they have recently cofounded REGAIN Therapeutics, owner of a patent application that covers synthetic soluble non-aggregating peptide analogues as replacement treatment in proteinopathies.
About this Alzheimer’s disease research news
Source: University of Cincinnati
Contact: Angela Koenig – University of Cincinnati
Image: The image is credited to Life Science Animation
Original Research: Open access.
“High cerebrospinal amyloid-β 42 is associated with normal cognition in individuals with brain amyloidosis” by Alberto Espay et al. EClinicalMedicine
Abstract
High cerebrospinal amyloid-β 42 is associated with normal cognition in individuals with brain amyloidosis
Background
Brain amyloidosis does not invariably predict dementia. We hypothesized that high soluble 42-amino acid β amyloid (Aβ42) peptide levels are associated with normal cognition and hippocampal volume despite increasing brain amyloidosis.
Methods
This cross-sectional study of 598 amyloid-positive participants in the Alzheimer’s Disease Neuroimaging Initiative cohort examined whether levels of soluble Aβ42 are higher in amyloid-positive normal cognition (NC) individuals compared to mild cognitive impairment (MCI) and Alzheimer’s disease (AD) and whether this relationship applies to neuropsychological assessments and hippocampal volume measured within the same year. All subjects were evaluated between June 2010 and February 2019. Brain amyloid positivity was defined as positron emission tomography-based standard uptake value ratio (SUVR) ≥1.08 for [18] F-florbetaben or 1.11 for [18]F-florbetapir, with higher SUVR indicating more brain amyloidosis. Analyses were adjusted for age, sex, education, APOE4, p-tau, t-tau, and centiloids levels.
Findings
Higher soluble Aβ42 levels were observed in NC (864.00 pg/ml) than in MCI (768.60 pg/ml) or AD (617.46 pg/ml), with the relationship between NC, MCI, and AD maintained across all amyloid tertiles. In adjusted analysis, there was a larger absolute effect size of soluble Aβ42 than SUVR for NC (0.82 vs. 0.40) and MCI (0.60 vs. 0.26) versus AD. Each standard deviation increase in Aβ42 was associated with greater odds of NC than AD (adjusted odds ratio, 6.26; p < 0.001) or MCI (1.42; p = 0.006). Higher soluble Aβ42 levels were also associated with better neuropsychological function and larger hippocampal volume.
Interpretation
Normal cognition and hippocampal volume are associated with preservation of high soluble Aβ42 levels despite increasing brain amyloidosis.