Summary: Deep sleep may clear the brain of toxic waste via a process driven by norepinephrine, a molecule that creates rhythmic blood vessel contractions. This “brainwashing” system, part of the glymphatic system, helps remove harmful proteins linked to neurological disorders.
Researchers found that sleep aids like zolpidem might impair this process by reducing norepinephrine waves, potentially disrupting brain waste clearance. The study underscores the importance of restorative sleep and its role in preventing cognitive decline.
Key Facts
- Glymphatic Function: Deep sleep facilitates waste removal in the brain, clearing harmful proteins through the glymphatic system.
- Norepinephrine Waves: During deep sleep, norepinephrine drives rhythmic blood vessel contractions, propelling brain fluid to remove waste.
- Sleep Aid Impact: Sleep medications like zolpidem may reduce norepinephrine waves, disrupting the brain’s cleaning process by 30%.
Source: Cell Press
A good night’s sleep does more than just help you feel rested—it might literally clear your mind.
A new study published January 8 in the Cell Press journal Cell shows how deep sleep may wash away waste buildup in the brain during waking hours, an essential process for maintaining brain health.
The findings also offer insights into how sleep aids may disrupt the “brainwashing” system, potentially affecting cognitive function in the long run.
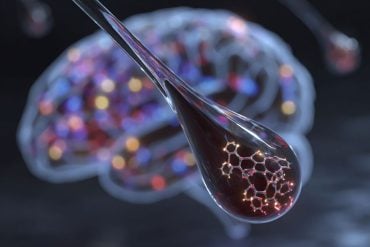
Scientists have known that the brain has a built-in waste removal system, called the glymphatic system, which circulates fluid in the brain and spinal cord to clear out waste.
This process helps remove toxic proteins that form sticky plaques linked to neurological disorders. However, what drives this system has remained unclear, until now.
Danish scientists found that a molecule called norepinephrine plays a key role in the brain’s cleaning in mice. During deep sleep, the brainstem releases tiny waves of norepinephrine about once every 50 seconds.
Norepinephrine triggers blood vessels to contract, generating slow pulsations that create a rhythmic flow in the surrounding fluid to carry waste away.
“It’s like turning on the dishwasher before you go to bed and waking up with a clean brain,” says senior author Maiken Nedergaard of the University of Rochester and University of Copenhagen, Denmark.
“We’re essentially asking what drives this process and trying to define restorative sleep based on glymphatic clearance.”
To find clues, Nedergaard and her team looked into what happens in mice when the brain sleeps. Specifically, they focused on the relationship between norepinephrine and blood flow during deep slumber.
They found that norepinephrine waves correlate to variations in brain blood volume, suggesting norepinephrine triggers a rhythmic pulsation in the blood vessels.
The team then compared the changes in blood volume to brain fluid flow. They found that the brain fluid flow fluctuates in correspondence to blood volume changes, suggesting that the vessels act as pumps to propel the surrounding brain fluid to flush out waste.
“You can view norepinephrine as this conductor of an orchestra,” says lead author Natalie Hauglund of the University of Copenhagen and the University of Oxford, UK.
“There’s a harmony in the constriction and dilation of the arteries, which then drives the cerebrospinal fluid through the brain to remove the waste products.”
Hauglund then had another question—is all sleep created equal? To find out, the researchers gave mice zolpidem, a common drug to aid sleep. They found that the norepinephrine waves during deep sleep was 50% lower in zolpidem-treated mice than in naturally sleeping mice.
Although the zolpidem-treated mice fell asleep faster, fluid transport into the brain dropped more than 30%. The findings suggest that the sleeping aid may disrupt the norepinephrine-driven waste clearance during sleep.
“More and more people are using sleep medication, and it’s really important to know if that’s healthy sleep,” says Hauglund.
“If people aren’t getting the full benefits of sleep, they should be aware of that so they can make informed decisions.”
The team says that the findings likely apply to humans, who also have a glymphatic system, although this needs further testing. Researchers have observed similar norepinephrine waves, blood flow patterns, and brain fluid flux in humans.
Their findings may offer insights into how poor sleep may contribute to neurological disorders like Alzheimer’s disease.
“Now we know norepinephrine is driving the cleaning of the brain, we may figure out how to get people a long and restorative sleep,” says Nedergaard.
Funding:
This work was supported by the Lundbeck Foundation, the Novo Nordisk Foundation, the National Institutes of Health, the US Army Research Office, the Human Frontier Science Program, the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the Simons Foundation, the Cure Alzheimer Fund, the Danmarks Frie Forskningsfond, and JPND/Good Vibes.
About this sleep and cognition research news
Author: Kristopher Benke
Source: Cell Press
Contact: Kristopher Benke – Cell Press
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Norepinephrine-mediated slow vasomotion drives glymphatic clearance during sleep” by Maiken Nedergaard et al. Cell
Abstract
Norepinephrine-mediated slow vasomotion drives glymphatic clearance during sleep
As the brain transitions from wakefulness to sleep, processing of external information diminishes while restorative processes, such as glymphatic removal of waste products, are activated. Yet, it is not known what drives brain clearance during sleep.
We here employed an array of technologies and identified tightly synchronized oscillations in norepinephrine, cerebral blood volume, and cerebrospinal fluid (CSF) as the strongest predictors of glymphatic clearance during NREM sleep.
Optogenetic stimulation of the locus coeruleus induced anti-correlated changes in vasomotion and CSF signal. Furthermore, stimulation of arterial oscillations enhanced CSF inflow, demonstrating that vasomotion acts as a pump driving CSF into the brain.
On the contrary, the sleep aid zolpidem suppressed norepinephrine oscillations and glymphatic flow, highlighting the critical role of norepinephrine-driven vascular dynamics in brain clearance.
Thus, the micro-architectural organization of NREM sleep, driven by norepinephrine fluctuations and vascular dynamics, is a key determinant for glymphatic clearance.