Summary: Neuroimaging study reveals significant brain changes in areas associated with language comprehension, cognition, and circadian rhythm control six months after COVID-19 infection.
Source: RSNA
Using a special type of MRI, researchers have uncovered brain changes in patients up to six months after they recovered from COVID-19, according to a study being presented next week at the annual meeting of the Radiological Society of North America (RSNA).
About one in five adults will develop long-term effects from COVID-19, according to the U.S. Centers for Disease Control and Prevention. Neurological symptoms associated with long COVID include difficulty thinking or concentrating, headache, sleep problems, lightheadedness, pins-and-needles sensation, change in smell or taste, and depression or anxiety. However, studies have found that COVID-19 may be associated with changes to the heart, lungs or other organs even in asymptomatic patients.
As more people become infected and recover from COVID-19, research has begun to emerge, focusing on the lasting consequences of the disease.
For this study, researchers used susceptibility-weighted imaging to analyze the effects that COVID-19 has on the brain. Magnetic susceptibility denotes how much certain materials, such as blood, iron and calcium, will become magnetized in an applied magnetic field. This ability aids in the detection and monitoring of a host of neurologic conditions including microbleeds, vascular malformations, brain tumors and stroke.
“Group-level studies have not previously focused on COVID-19 changes in magnetic susceptibility of the brain despite several case reports signaling such abnormalities,” said study co-author Sapna S. Mishra, a Ph.D. candidate at the Indian Institute of Technology in Delhi. “Our study highlights this new aspect of the neurological effects of COVID-19 and reports significant abnormalities in COVID survivors.”
The researchers analyzed the susceptibility-weighted imaging data of 46 COVID-recovered patients and 30 healthy controls. Imaging was done within six months of recovery. Among patients with long COVID, the most commonly reported symptoms were fatigue, trouble sleeping, lack of attention and memory issues.
“Changes in susceptibility values of brain regions may be indicative of local compositional changes,” Mishra said. “Susceptibilities may reflect the presence of abnormal quantities of paramagnetic compounds, whereas lower susceptibility could be caused by abnormalities like calcification or lack of paramagnetic molecules containing iron.”
MRI results showed that patients who recovered from COVID-19 had significantly higher susceptibility values in the frontal lobe and brain stem compared to healthy controls. The clusters obtained in the frontal lobe primarily show differences in the white matter.
“These brain regions are linked with fatigue, insomnia, anxiety, depression, headaches and cognitive problems,” Mishra said.
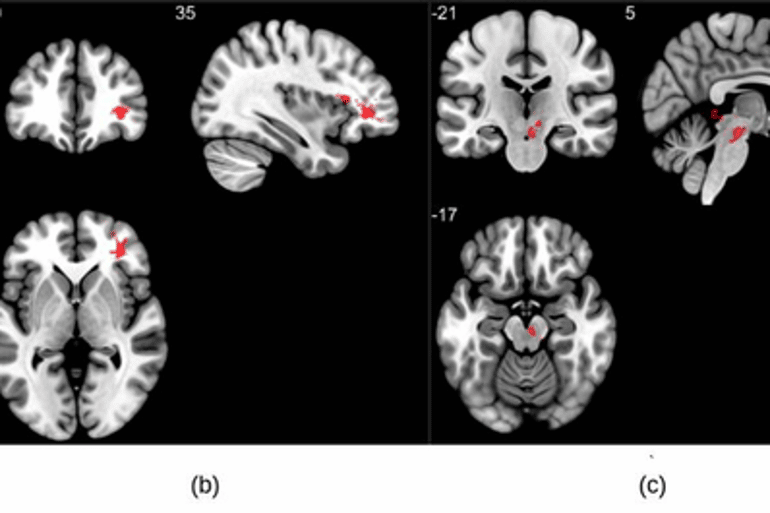
Portions of the left orbital-inferior frontal gyrus (a key region for language comprehension and production) and right orbital-inferior frontal gyrus (associated with various cognitive functions including attention, motor inhibition and imagery, as well as social cognitive processes) and the adjacent white matter areas made up the frontal lobe clusters.
The researchers also found a significant difference in the right ventral diencephalon region of the brain stem. This region is associated with many crucial bodily functions, including coordinating with the endocrine system to release hormones, relaying sensory and motor signals to the cerebral cortex and regulating circadian rhythms (the sleep-wake cycle).
“This study points to serious long-term complications that may be caused by the coronavirus, even months after recovery from the infection,” Mishra said. “The present findings are from the small temporal window. However, the longitudinal time points across a couple of years will elucidate if there exists any permanent change.”
The researchers are conducting a longitudinal study on the same patient cohort to determine whether these brain abnormalities persist over a longer time frame.
Co-authors are Rakibul Hafiz, Ph.D., Tapan Gandhi, Ph.D., Vidur Mahajan, M.B.B.S., Alok Prasad, M.D., and Bharat Biswal, Ph.D.
About this neurology and COVID-19 research news
Author: Linda Brooks
Source: RSNA
Contact: Linda Brooks – RSNA
Image: The image is credited to RSNA and Sapna S. Mishra
Original Research: The findings will be presented at the 108th Scientific Assembly and Annual Meeting of the Radiological Society of North America







