New research from Karolinska Institutet shows that hypersexual disorder – known popularly as sex addiction – can be linked to hyperactive stress systems. In a stress regulation test using the cortisone drug dexamethasone, men with hypersexual disorder showed higher levels of stress hormones than controls, a finding that the researchers hope will contribute to improved therapy for this patient group. The results are published in the journal Psychoneuroendocrinology.
Hypersexual disorder, or an overactive sex drive, normally entails obsessive thoughts of sex, a compulsion to perform sexual acts, a loss of control, or sexual habits that carry potential problems or risks. The diagnosis is not uncontroversial, however, since there is often co-morbidity with another kind of mental health issue.
Psychiatrist and researcher Jussi Jokinen has spent many years trying to find the neurobiological causes of mental illness. In the present study, he and his group at Karolinska Institutet’s Department of Clinical Neuroscience have used what is known as a dexamethasone test to measure the patients’ stress systems. Dexamethasone is a cortisone drug used for depressing the immune system, such as during an anaphylactic shock or an organ transplant; it also serves, however, as a kind of chemical stress test.
The study involved 67 men with hypersexual disorder and 39 healthy matched controls. The participants were carefully diagnosed for hypersexual disorder and any co-morbidity with depression or childhood trauma. The researchers gave them a low dose of dexamethasone on the evening before the test to inhibit their physiological stress response, and then in the morning measured their levels of stress hormones cortisol and ACTH. They found that patients with hypersexual disorder had higher levels of such hormones than the healthy controls, a difference that remained even after controlling for co-morbid depression and childhood trauma.
Childhood trauma
“Aberrant stress regulation has previously been observed in depressed and suicidal patients as well as in substance abusers,” says Professor Jokinen. “In recent years, the focus has been on whether childhood trauma can lead to a dysregulation of the body’s stress systems via so-called epigenetic mechanisms, in other words how their psychosocial environments can influence the genes that control these systems.”
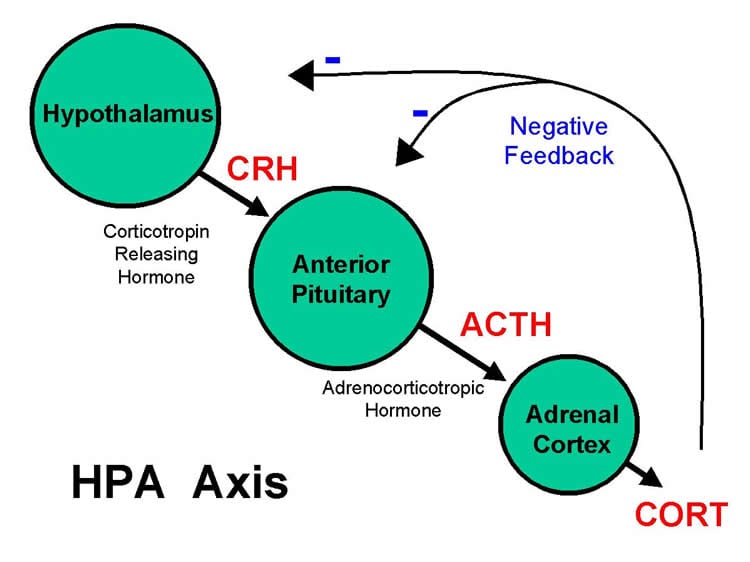
According to the researchers, the results suggest that the same neurobiological system involved in another type of abuse can apply to people with hypersexual disorder. The next step is to see if the psychotherapy given the patients has helped to normalise their physiological stress response. They also plan to perform epigenetic analyses.
“This is the first study of neurobiological disorders in this particular patient group,” says Professor Jokinen. “It’s important to study stress systems in patients with different psychiatric diagnoses in order to understand if these biological changes are diagnosis-specific or related to different behaviours, and to take into account the impact that childhood trauma has on later mental health.”
The study’s first author was Andreas Chatzittofis, psychiatrist and doctoral student at Karolinska Institutet’s Department of Clinical Neuroscience. The patients were recruited from the Centre for Andrology and Sexual Medicine at Karolinska University Hospital, Huddinge, through the cooperation of consultant and Associate Professor Dr Stefan Arver and psychologist Katarina Görts Öberg,PhD. Jussi Jokinen is also Professor of psychiatry at the Department of Clinical Science at Umeå University.
Funding: The study was financed with a grant from the Swedish Research Council and through the ALF grant agreement between Stockholm County Council and Karolinska Institutet.
Source: Karolinska Institute
Image Credit: The image is in the public domain
Original Research: Abstract for “HPA axis dysregulation in men with hypersexual disorder” by Chatzittofis A, Arver S, Öberg K, Hallberg J, Nordström P, and Jokinen J in Psychoneuroendocrinology. Published online October 7 2015 doi:10.1016/j.psyneuen.2015.10.002
Abstract
HPA axis dysregulation in men with hypersexual disorder
Hypersexual disorder integrating pathophysiological aspects such as sexual desire deregulation, sexual addiction, impulsivity and compulsivity was suggested as a diagnosis for the DSM-5. However, little is known about the neurobiology behind this disorder. A dysregulation of the hypothalamic pituitary adrenal (HPA) axis has been shown in psychiatric disorders but has not been investigated in hypersexual disorder. The aim of this study was to investigate the function of the HPA axis in hypersexual disorder.
The study includes 67 male patients with hypersexual disorder and 39 healthy male volunteers. Basal morning plasma levels of cortisol and ACTH were assessed and low dose (0.5 mg) dexamethasone suppression test was performed with cortisol and ACTH measured post dexamethasone administration. Non-suppression status was defined with DST-cortisol levels ≥138 nmol/l. The Sexual Compulsive scale (SCS), Hypersexual disorder current assessment scale (HD:CAS), Montgomery-Åsberg Depression Scale-self rating (MADRS-S) and Childhood trauma questionnaire (CTQ), were used for assessing hypersexual behavior, depression severity and early life adversity.
Patients with hypersexual disorder were significantly more often DST non-suppressors and had significantly higher DST-ACTH levels compared to healthy volunteers. The patients reported significantly more childhood trauma and depression symptoms compared to healthy volunteers. CTQ scores showed a significant negative correlation with DST-ACTH whereas SCS and HD:CAS scores showed a negative correlation with baseline cortisol in patients. The diagnosis of hypersexual disorder was significantly associated DST non-suppression and higher plasma DST-ACTH even when adjusted for childhood trauma.
The results suggest HPA axis dysregulation in male patients with hypersexual disorder.
“HPA axis dysregulation in men with hypersexual disorder” by Chatzittofis A, Arver S, Öberg K, Hallberg J, Nordström P, and Jokinen J in Psychoneuroendocrinology. Published online October 7 2015 doi:10.1016/j.psyneuen.2015.10.002