Summary: Heart disease that causes brain dysfunction can lead to the development of Alzheimer’s disease and triples the amount of amyloid-beta in the brain.
Source: University of Sheffield
Heart disease can directly cause brain dysfunction early on which could lead to dementia and can treble the amount of an Alzheimer’s protein in the brain, say scientists.
The new research, published in eLife, has found that heart disease causes a breakdown of a key brain function which links brain activity and blood flow, meaning the brain gets less blood for the same amount of activity.
This is happening in heart disease patients before the build up of fat in the brain’s blood vessels (atherosclerosis) and is a prelude to dementia. Until now it has been unclear how some forms of vascular dementia can happen years before atherosclerosis in the brain.
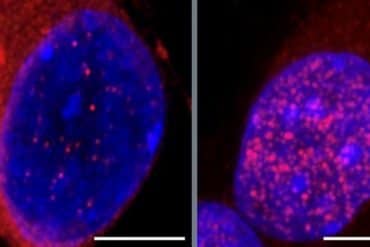
The researchers also discovered that the combination of heart disease and a genetic predisposition for Alzheimer’s Disease trebles the amount of beta-amyloid, a protein that builds up and triggers Alzheimer’s, and increases the levels of an inflammatory gene (IL1) in the brain.
Dr Osman Shabir, lead author of the study from the University of Sheffield’s Neuroscience and Healthy Lifespan Institutes, said: “Alzheimer’s Disease is the most common form of dementia worldwide and heart disease is a major risk factor for both Alzheimer’s and dementia. The new findings are key to furthering our understanding of the links between heart disease and dementia.
“We’ve discovered that heart disease in midlife causes the breakdown of neurovascular coupling, an important mechanism in our brains which controls the amount of blood supplied to our neurons. This breakdown means the brain doesn’t get enough oxygen when needed and in time this can lead to dementia.”
The team have since been awarded a three year grant by the British Heart Foundation to look at the use of an arthritis drug which targets IL1 to see if it could reverse or reduce the brain dysfunction seen to be caused by heart disease.
The team also found that brain injuries can also worsen brain blood flow regulation, supporting observations that patients’ symptoms often worsen after injuries or falls.
About this Alzheimer’s disease research news
Author: Emma Griffiths
Source: University of Sheffield
Contact: Emma Griffiths – University of Sheffield
Image: The image is in the public domain
Original Research: Open access.
“Assessment of neurovascular coupling and cortical spreading depression in mixed mouse models of atherosclerosis and Alzheimer’s disease” by Osman Shabir et al. eLife
Abstract
Assessment of neurovascular coupling and cortical spreading depression in mixed mouse models of atherosclerosis and Alzheimer’s disease
Neurovascular coupling is a critical brain mechanism whereby changes to blood flow accompany localised neural activity. The breakdown of neurovascular coupling is linked to the development and progression of several neurological conditions including dementia.
In this study, we examined cortical haemodynamics in mouse preparations that modelled Alzheimer’s disease (J20-AD) and atherosclerosis (PCSK9-ATH) between 9 and 12 m of age.
We report novel findings with atherosclerosis where neurovascular decline is characterised by significantly reduced blood volume, altered levels of oxyhaemoglobin and deoxyhaemoglobin, in addition to global neuroinflammation. In the comorbid mixed model (J20-PCSK9-MIX), we report a 3 x increase in hippocampal amyloid-beta plaques. A key finding was that cortical spreading depression (CSD) due to electrode insertion into the brain was worse in the diseased animals and led to a prolonged period of hypoxia.
These findings suggest that systemic atherosclerosis can be detrimental to neurovascular health and that having cardiovascular comorbidities can exacerbate pre-existing Alzheimer’s-related amyloid-plaques.