Summary: Speaking without a facemask in confined spaces poses the biggest risk for spreading SARS_CoV_2, the virus responsible for COVID-19.
Source: Wiley
A new review published in the Journal of Internal Medicine indicates that unmasked speech in confined spaces poses the greatest risk of spreading SARS-CoV-2, the virus that causes COVID-19, to others.
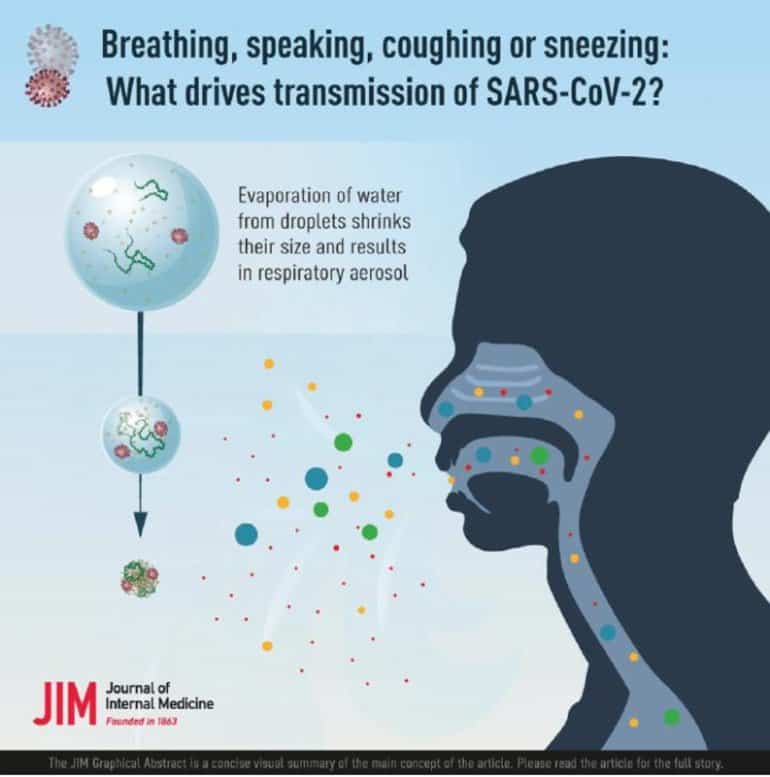
The focus of the review is on the interface between physics and medicine, and it describes how different sized respiratory droplets emitted while speaking span a continuum of sizes and can carry different amounts of virus.
Most concerning are intermediate-sized droplets that remain suspended in air for minutes and can be transported over considerable distances by convective air currents.
“We’ve all seen some spit droplets flying when people talk but there are thousands more, too small to be seen by the naked eye. When the water evaporates from such speech-generated, potentially virus-rich droplets, they float in the air for minutes, like smoke, thus putting others at risk,” said senior author Adriaan Bax, PhD, of the National Institute of Diabetes and Digestive and Kidney Diseases.
About this COVID-19 research news
Source: Wiley
Contact: Press Office – Wiley
Image: The image is credited to Journal of Internal Medicine
Original Research: Open access.
“Breathing, speaking, coughing or sneezing: What drives transmission of SARS-CoV-2?” by Adriaan Bax et al. Journal of Internal Medicine
Abstract
Breathing, speaking, coughing or sneezing: What drives transmission of SARS-CoV-2?
The SARS-CoV-2 virus is highly contagious, as demonstrated by numerous well-documented superspreading events. The infection commonly starts in the upper respiratory tract (URT) but can migrate to the lower respiratory tract (LRT) and other organs, often with severe consequences.
Whereas LRT infection can lead to shedding of virus via breath and cough droplets, URT infection enables shedding via abundant speech droplets. Their viral load can be high in carriers with mild or no symptoms, an observation linked to the abundance of SARS-CoV-2-susceptible cells in the oral cavity epithelium. Expelled droplets rapidly lose water through evaporation, with the smaller ones transforming into long-lived aerosol.
Although the largest speech droplets can carry more virions, they are few in number, fall to the ground rapidly and therefore play a relatively minor role in transmission. Of more concern is small speech aerosol, which can descend deep into the LRT and cause severe disease. However, since their total volume is small, the amount of virus they carry is low.
Nevertheless, in closed environments with inadequate ventilation, they can accumulate, which elevates the risk of direct LRT infection. Of most concern is the large fraction of speech aerosol that is intermediate-sized because it remains suspended in air for minutes and can be transported over considerable distances by convective air currents.
The abundance of this speech-generated aerosol, combined with its high viral load in pre- and asymptomatic individuals, strongly implicates airborne transmission of SARS-CoV-2 through speech as the primary contributor to its rapid spread.






