Summary: Tissue in specific brain areas increases in patients with psychosis, even before they receive treatment.
Source: University of Western Ontario
A new study from Western’s Schulich School of Medicine & Dentistry and collaborators from West China Hospital in Chengdu, is challenging long-held notions about brain deterioration in patients with psychotic disorders, and may help improve treatment protocols.
Psychotic disorders such as psychosis are often characterized as progressively worsening, with the brain deteriorating as the condition recurs through time.
The study, led by Dr. Lena Palaniyappan, psychiatry professor and scientist at Robarts Research Institute, showed brain tissue actually increases in certain areas in patients with psychosis—even before they receive treatment.
This could indicate that the brain’s attempts to rebuild itself may start even before a patient receives medical , Palaniyappan said.
Studying this phenomenon further may help researchers improve treatment protocols and eventually have impacts on how we view and treat other youth-onset mental disorders.
“When a young person develops psychosis, their family often fears what will happen in the future,” explained Palaniyappan. “It’s usually not a single episode. There’s a high chance people will continue to be unwell, and relapse is likely.”
It’s that aspect of the disorder—the ongoing recurrence of episodes of psychosis—that Palaniyappan said contributes to the view of the illness as progressive.
“Things do go downhill after psychosis first hits,” he said. “For 150 years, our conception of psychosis is that there is a lot of evidence to support the idea of deterioration through time.”
But what does the brain do to recover? That’s the key question Palaniyappan sought to answer.
“The brain is not passive, but a plastic organ—it tries to combat, to some extent, the trauma and stress inflicted by psychiatric conditions,” he explained.
Palaniyappan’s team studied people with psychosis before they started receiving treatment to better understand how the brain responds.
For 11 years, the team examined 340 patients who had not yet received any anti-psychotic medications at a partner hospital in West China—and made a remarkable discovery.
While the team’s results did confirm a reduction in brain tissue in patients with psychosis compared to healthy people—even before receiving any treatment—they also observed increases in brain tissue in several parts of the brain, with correlations to better patient outcomes.
“The higher the increase, the better some of the outcomes are,” Palaniyappan said. “The symptoms are less severe, duration of illness is shorter, and those with more increases in brain tissue perform better in cognitive tasks.”
The results show two major findings: First, before medical intervention, the brain may already be attempting to reduce the impact of psychosis. Second, this rebuilding process may not be enough to fully stave off the disorder.
“What this finding suggests is that psychosis is not a condition like dementia, where brain changes are degenerative, without any evidence of a reversal,” Palaniyappan said. “There are reversals already happening in the brain, to a small extent, by the time a person knocks at a doctor’s door with psychosis. If we can understand why and how this occurs, we may be able to improve it.”
However, Palaniyappan said this study does not offer experimental proof and is limited by the fact that only one brain scan was obtained from each patient. While researchers do not know if the observed changes persist over time, the discovery opens the door to looking at psychosis treatments in a different way.
“Most of the research to find new therapeutics and interventions in psychosis depend on the framework that the brain changes are signs of a damage,” he said. “If we shift our focus from brain damage and understand the mechanisms behind the brain’s attempts to recover and compensate, maybe we can achieve better outcomes.”
Another important clue in the future of psychosis treatment is that about one in six patients will only ever have one psychotic episode in their lifetime, but it remains unclear why and there’s no way to predict who that might be.
“Most severe psychiatric disorders, about 75 percent, start in teens or pre-teens and then become a life-spanning illness,” he said. “Almost all of the treatments we have are only symptom control measures; they are not curative. We do not know how to reverse the underlying processes.”
As next steps, Palaniyappan said his team can look at replicating these studies in other large-scale samples. Studies in animal models to attempt to induce changes in brain tissue could also play a role in better understanding the brain’s compensation process.
“Understanding compensatory processes will open the door to new ways of addressing many mental health problems,” he said.
About this psychosis research news
Author: Max Martin
Source: University of Western Ontario
Contact: Max Martin – University of Western Ontario
Image: The image is credited to University of Western Ontario
Original Research: Closed access.
“Ameliorative patterns of grey matter in patients with first-episode and treatment-naïve schizophrenia” by Mingli Li et al. Psychological Medicine
Abstract
Ameliorative patterns of grey matter in patients with first-episode and treatment-naïve schizophrenia
Background
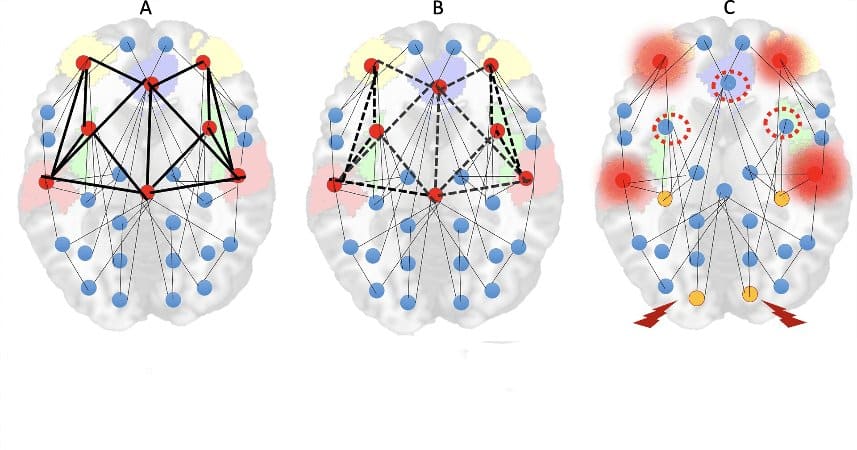
Grey matter (GM) reduction is a consistent observation in established late stages of schizophrenia, but patients in the untreated early stages of illness display an increase as well as a decrease in GM distribution relative to healthy controls (HC). The relative excess of GM may indicate putative compensatory responses, though to date its relevance is unclear.
Methods
343 first-episode treatment-naïve patients with schizophrenia (FES) and 342 HC were recruited. Multivariate source-based morphometry was performed to identify covarying ‘networks’ of grey matter concentration (GMC). Neurocognitive scores using the Cambridge Neuropsychological Test Automated Battery (CANTAB) and symptom burden using the Positive and Negative Symptoms Scale (PANSS) were obtained. Bivariate linear relationships between GMC and cognition/symptoms were studied.
Results
Compared to healthy subjects, FES had prominently lower GMC in two components; the first consists of the anterior insula, inferior frontal gyrus, anterior cingulate and the second component with the superior temporal gyrus, precuneus, inferior/superior parietal lobule, cuneus, and lingual gyrus. Higher GMC was seen in adjacent areas of the middle and superior temporal gyrus, middle frontal gyrus, inferior parietal cortex and putamen. Greater GMC of this component was associated with lower duration of untreated psychosis, less severe positive symptoms and better performance on cognitive tests.
Conclusions
In untreated stages of schizophrenia, both a distributed lower and higher GMC is observable. While the higher GMC is relatively modest, it occurs across frontoparietal, temporal and subcortical regions in association with reduced illness burden suggesting a compensatory role for higher GMC in the early stages of schizophrenia.