Summary: Researchers made a significant discovery regarding microglia, the immune cells of the central nervous system, and their role in neurodegenerative diseases. They investigated how these cells respond to injury and their change in behavior under specific conditions.
Notably, the researchers found that microglia in models of Multiple Sclerosis (MS) displayed similar characteristics to those seen in Alzheimer’s disease. This research could pave the way for novel strategies to protect the human brain when microglia become neurotoxic.
Key Facts:
- Microglia are immune cells of the central nervous system that can both protect and potentially harm the brain and spinal cord.
- The University of Alberta study found similarities between microglia in MS and Alzheimer’s disease models, suggesting similar mechanisms could be at work.
- The research aims to identify toxic properties of neurotoxic microglia, which could lead to new methods of protecting the brain from neurodegenerative diseases.
Source: University of Alberta
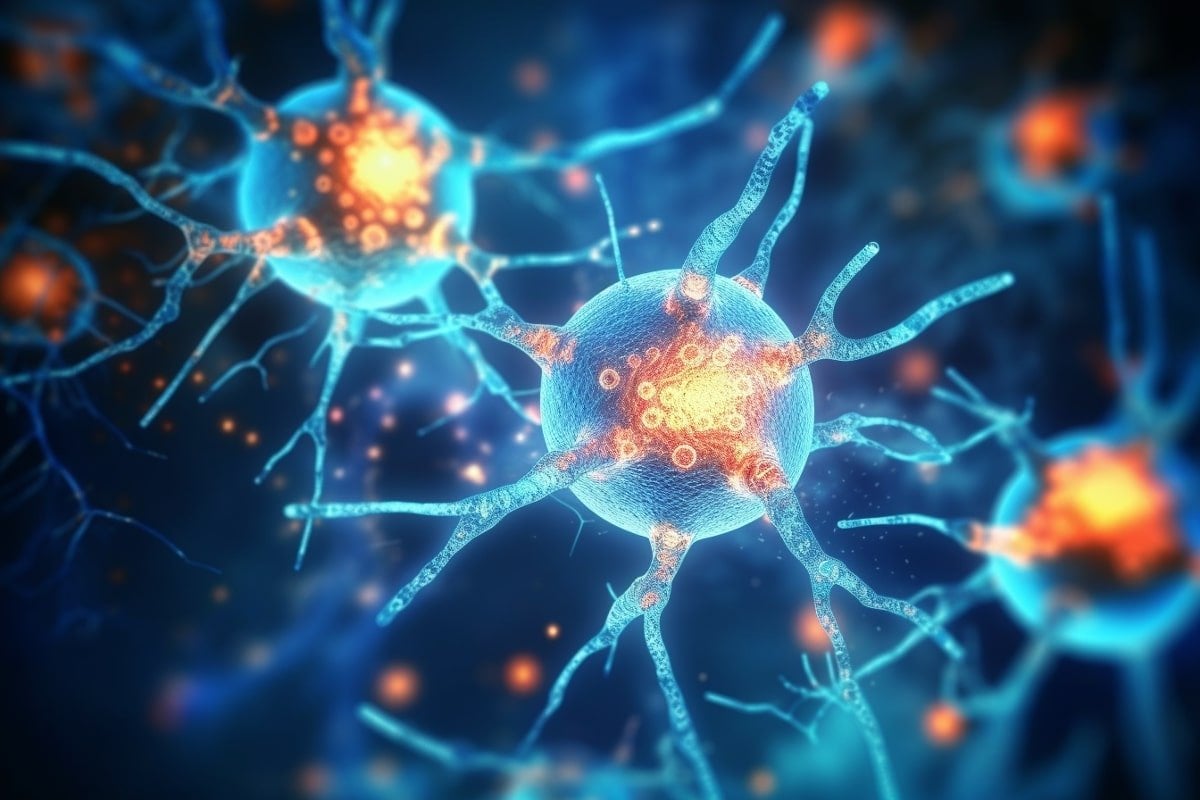
In the human central nervous system, there are tiny cells that—for most people, most of the time—provide important immune protection to the brain and spinal cord. Occasionally these microglia cells run terribly awry, leading to neurodegenerative diseases like multiple sclerosis and Alzheimer’s disease.
But in a recent study, University of Alberta researchers have found new information about how these immune cells change and respond to injury—a discovery that could help in the search for ways to protect the human brain when these cells go bad.
“We know that under certain conditions the microglia are profoundly important for regeneration—and we also know that under other conditions they may have seemingly neurotoxic properties,” says Jason Plemel, assistant professor of neurology in the Faculty of Medicine & Dentistry and Canada Research Chair in Glial Neuroimmunology.
Plemel and his team are searching for ways to direct the central nervous system’s immune response to minimize further damage.
“Our lab is studying the yin and yang of microglia—we’re really trying to understand if and how the microglia become neurotoxic.”
Understanding immune cell behavior
In the study, Plemel’s laboratory was trying to find out how microglia behave when demyelination—that is, damage to the myelin, or insulating material that coats most neurons—is chemically induced in animal models. Multiple sclerosis is a demyelinating disease.
Previous research has shown that microglia play a large role in demyelination. In fact, in this type of model, from the earliest stages, if you get rid of microglia throughout, no demyelination occurs.
But that’s only part of the story, Plemel explains, because the role of microglia is complex.
“We saw that when we remove microglia in later stages, there is no change in demyelination. And microglia are almost exclusively responding to the injury and behave in the way we would think immune cells respond. They consume debris and lytic cells, cells that died in an inflammatory way, in this diseased model,” says Plemel.
In the study, the researchers also compared the microglia in the MS injury model with those that had been described in previous research on an Alzheimer’s disease model and found that “they look very similar,” according to Plemel.
“This tells us that the microglia immune cells present in MS white-matter injury have similar characteristic states and functions to the ones in Alzheimer’s disease,” he notes.
Pointing the way toward treatments
Plemel says it has been generally accepted that the immune cells can be neurotoxic but he doesn’t think that has been fully proven. By continuing in-depth study of the microglia, he hopes to be able to identify toxic attributes or properties—and “maybe make neurotoxic microglia less injurious.”
“What it means for people with MS is that if their brains’ immune cells were to become toxic under certain conditions, then this research could open up a new way to protect their brains against damage.”
About this neuroscience research news
Author: Ramona Czakert Franson
Source: University of Alberta
Contact: Ramona Czakert Franson – University of Alberta
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Single-cell microglial transcriptomics during demyelination defines a microglial state required for lytic carcass clearance” by Sameera Zia et al. Molecular Neurodegeneration
Abstract
Single-cell microglial transcriptomics during demyelination defines a microglial state required for lytic carcass clearance
Background
Microglia regulate the response to injury and disease in the brain and spinal cord. In white matter diseases microglia may cause demyelination. However, how microglia respond and regulate demyelination is not fully understood.
Methods
To understand how microglia respond during demyelination, we fed mice cuprizone—a potent demyelinating agent—and assessed the dynamics of genetically fate-mapped microglia. We then used single-cell RNA sequencing to identify and track the microglial subpopulations that arise during demyelination. To understand how microglia contribute to the clearance of dead oligodendrocytes, we ablated microglia starting at the peak of cuprizone-induced cell death and used the viability dye acridine orange to monitor apoptotic and lytic cell morphologies after microglial ablation. Lastly, we treated serum-free primary microglial cultures to model distinct aspects of cuprizone-induced demyelination and assessed the response.
Results
The cuprizone diet generated a robust microglial response by week 4 of the diet. Single-cell RNA sequencing at this time point revealed the presence of several cuprizone-associated microglia (CAM) clusters. These clusters expressed a transcriptomic signature indicative of cytokine regulation and reactive oxygen species production with altered lysosomal and metabolic changes consistent with ongoing phagocytosis. Using acridine orange to monitor apoptotic and lytic cell death after microglial ablation, we found that microglia preferentially phagocytose lytic carcasses. In culture, microglia exposed to lytic carcasses partially recapitulated the CAM state, suggesting that phagocytosis contributes to this distinct microglial state during cuprizone demyelination.
Conclusions
Microglia serve multiple roles during demyelination, yet their transcriptomic state resembles other neurodegenerative conditions. The phagocytosis of cellular debris is likely a universal cause for a common neurodegenerative microglial state.