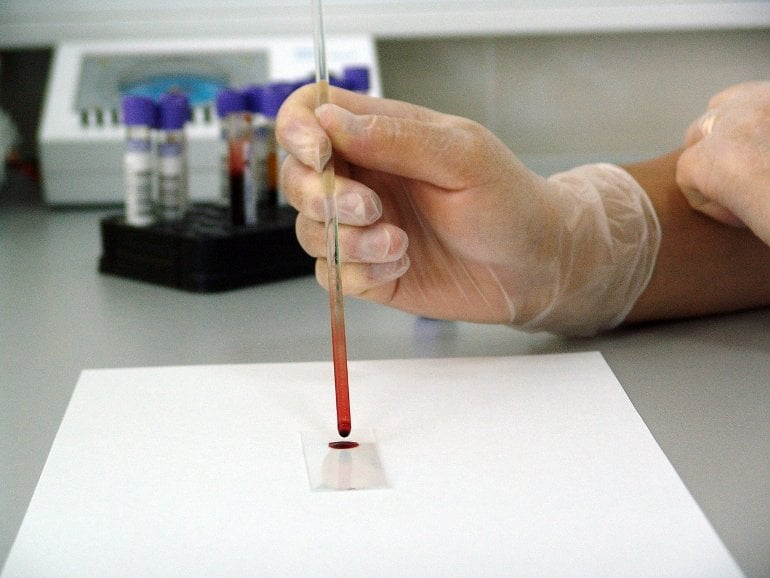
Summary: Researchers have developed a new blood test for brain-derived Tau that can follow and track the progression of Alzheimer’s disease while excluding other dementias.
Source: University of Gothenburg
A new blood test that can track and follow the neurodegeneration in Alzheimer’s disease – and exclude other dementias. That is an innovation now presented by researchers at the University of Gothenburg, together with colleagues in Italy and USA.
In recent years, a lot of effort has been put on developing biomarkers in blood that could potentially help to diagnose and monitor Alzheimer’s disease (AD). Tau – one of the main proteins involved in AD pathology – has been the focus of extensive research in the biomarker field.
The new blood-based phosphorylated tau markers for AD that have appeared in the last couple of years have proven that it is possible to have an accessible and effective test to screen patients with suspected Alzheimer’s disease.
However, measuring brain proteins in blood is a major challenge even with current technologies. Scientists at the University of Gothenburg and their industry partners engineered a novel antibody that specifically targets tau isoforms originating from the brain, by taking advantage of the architectural differences in the structure of tau protein found in the brain versus peripheral sources.
Addresses an unmet need
This breakthrough has allowed them to develop a new blood test that specifically and selectively measures non-phosphorylated tau coming from the brain into the bloodstream. This innovation addresses an urgent unmet need; a blood test that tracks neurodegenerative changes specifically in Alzheimer’s disease but not in other dementias.
The new brain derived tau (BD-tau) assay showed robust and stable technical performances in blood. Clinically, there were strong correlations between BD-tau levels in blood and CSF, indicating that the assay was measuring brain tau. Thanks to a collaboration between Italy, USA, and Sweden, they measured BD-tau levels in blood samples from 609 patients.
In a cohort of individuals who had received autopsy-verified diagnosis, plasma BD-tau showed to be a marker of neurodegeneration that differentiated Alzheimer’s disease from non-Alzheimer dementias. Remarkably, plasma BD-tau, but not neurofilament light (NfL), correlated with amyloid plaque and tau tangle loads in the brains of these individuals, further showing its specificity to Alzheimer’s disease.
High accuracy to differentiate
To demonstrate the clinical utility of these results, the researchers studied two separate memory clinic cohorts where the participants had been given a diagnosis of Alzheimer’s disease, other dementias or controls. Again, plasma BD-tau had a high accuracy to differentiate Alzheimer’s disease from other dementias, also outperforming plasma NfL.
The results show that plasma BD-tau is a new blood-based biomarker that can distinguish between AD and other type of dementias, and unlike other blood-based biomarkers like NfL, BD-tau uniquely reflects the extent of neurodegeneration in patients with Alzheimer’s disease.
Ten years ago, the National Institutes on Aging and the Alzheimer’s Association of the USA proposed a framework to identify and stage the progress of Alzheimer’s disease using biological evidence.
This framework, referred to as the AT(N) model, focuses on biomarkers of amyloid (A), tau (T), and neurodegeneration (N), and it has been authenticated using cerebrospinal fluid (CSF) and neuroimaging biomarkers. The CSF AT(N) markers include amyloid-beta (Aβ42/40), phosphorylated-tau (p-tau), and total tau.
Quick and accessible blood test
However, it has not been possible to fully implement the AT(N) system using blood biomarkers. This is because an N marker that shows specificity to Alzheimer pathophysiology is lacking. Plasma BD-tau allows to complete the AT(N) scheme in blood as a true neurodegeneration marker that is specific to Alzheimer-type pathology.
From a research perspective BD-tau will be useful to understand neurodegenerative processes in Alzheimer’s disease and how these differ from those in other dementias. From a clinical perspective, BD-tau could easily be implemented as a quick and accessible blood test to diagnose and monitor disease progression in patients with AD.
About this Alzheimer’s disease research news
Author: Margareta Gustafsson Kubista
Source: University of Gothenburg
Contact: Margareta Gustafsson Kubista – University of Gothenburg
Image: The image is in the public domain
Original Research: Open access.
“Brain-derived tau: a novel blood-based biomarker for Alzheimer’s disease-type neurodegeneration” by Kaj Blennow et al. Brain
Abstract
Brain-derived tau: a novel blood-based biomarker for Alzheimer’s disease-type neurodegeneration
Blood-based biomarkers for amyloid beta and phosphorylated tau show good diagnostic accuracies and agreements with their corresponding CSF and neuroimaging biomarkers in the amyloid/tau/neurodegeneration [A/T/(N)] framework for Alzheimer’s disease.
However, the blood-based neurodegeneration marker neurofilament light is not specific to Alzheimer’s disease while total-tau shows lack of correlation with CSF total-tau. Recent studies suggest that blood total-tau originates principally from peripheral, non-brain sources.
We sought to address this challenge by generating an anti-tau antibody that selectively binds brain-derived tau and avoids the peripherally expressed ‘big tau’ isoform.
We applied this antibody to develop an ultrasensitive blood-based assay for brain-derived tau, and validated it in five independent cohorts (n = 609) including a blood-to-autopsy cohort, CSF biomarker-classified cohorts and memory clinic cohorts.
In paired samples, serum and CSF brain-derived tau were significantly correlated (rho = 0.85, P < 0.0001), while serum and CSF total-tau were not (rho = 0.23, P = 0.3364). Blood-based brain-derived tau showed equivalent diagnostic performance as CSF total-tau and CSF brain-derived tau to separate biomarker-positive Alzheimer’s disease participants from biomarker-negative controls.
Furthermore, plasma brain-derived tau accurately distinguished autopsy-confirmed Alzheimer’s disease from other neurodegenerative diseases (area under the curve = 86.4%) while neurofilament light did not (area under the curve = 54.3%).
These performances were independent of the presence of concomitant pathologies. Plasma brain-derived tau (rho = 0.52–0.67, P = 0.003), but not neurofilament light (rho = −0.14–0.17, P = 0.501), was associated with global and regional amyloid plaque and neurofibrillary tangle counts.
These results were further verified in two memory clinic cohorts where serum brain-derived tau differentiated Alzheimer’s disease from a range of other neurodegenerative disorders, including frontotemporal lobar degeneration and atypical parkinsonian disorders (area under the curve up to 99.6%).
Notably, plasma/serum brain-derived tau correlated with neurofilament light only in Alzheimer’s disease but not in the other neurodegenerative diseases. Across cohorts, plasma/serum brain-derived tau was associated with CSF and plasma AT(N) biomarkers and cognitive function.
Brain-derived tau is a new blood-based biomarker that outperforms plasma total-tau and, unlike neurofilament light, shows specificity to Alzheimer’s disease-type neurodegeneration. Thus, brain-derived tau demonstrates potential to complete the AT(N) scheme in blood, and will be useful to evaluate Alzheimer’s disease-dependent neurodegenerative processes for clinical and research purposes.