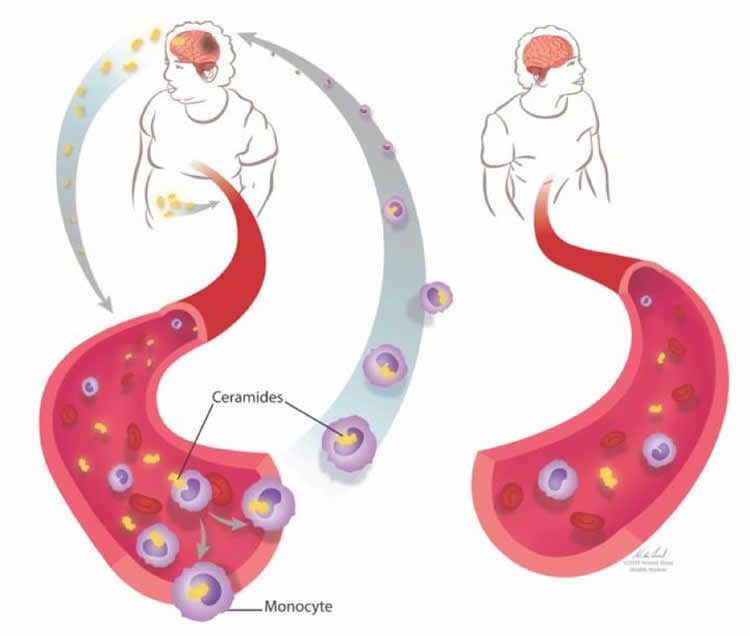
Summary: Obesity and a higher body mass index negatively impacts the progression of Multiple Sclerosis. Ceramides are more abundant in the blood of those who are overweight. The ceramides enter inside the nucleus of monocytes, causing proliferation. The increased number of monocytes travel back to the brain, causing more damage for those with RRMS.
Source: CUNY
A newly published paper in the Lancet journal EBioMedicine identifies a link between high levels of blood lipids and worsening of disease in multiple sclerosis (MS) patients who are overweight or obese.
The longitudinal investigation, conducted by researchers at the Advanced Science Research Center(ASRC) at The Graduate Center of The City University of New York’s Neuroscience Initiative in collaboration with clinicians at the Icahn School of Medicine at Mount Sinai, followed recently diagnosed MS patients for two years. The researchers found that individuals who were overweight or obese had higher levels of blood lipids called ceramides, which placed markers on the DNA of monocytes, making them proliferate. Monocytes are blood cells that can travel to the brain and damage nerve fibers, and two years into their diagnosis, study participants with higher levels of ceramides and monocytes also had greater loss of motor skills and more brain injury.
“Our study identifies important correlations between ceramide levels, body mass index, and disease progression in MS patients,” said ASRC Neuroscience Initiative Director Patrizia Casaccia, a professor at The Graduate Center.
“We found that overweight and obese individuals with MS have higher ceramide levels than people with the disease who are not overweight and also than individuals who are overweight or obese but otherwise in healthy conditions. This is important because we and others had previously identified ceramides in the cerebrospinal fluid surrounding the brain of MS patients, and we attributed their increased abundance to the body’s efforts to recycle the damaged myelin. In this study, however, we also detect higher ceramide levels in the blood of overweight and obese MS patients than we did in patients with normal body mass index, suggesting that overabundant lipids can be derived not only from damaged brain cells but also from excessive dietary intake of saturated fats.”
Methodology
Two cohorts of patients — a primary one and a validation group — were recruited from the Corinne Goldsmith Dickinson Center for Multiple Sclerosis at Mount Sinai and the National Institutes of Health to participate in the study. For the first group, 54 therapy-naïve MS patients 18 to 60 years old with high or normal body mass indexes (BMIs) were evaluated using brain MRI to identify signs of brain damage; a clinical assessment to ascertain weight, disabilities and other vital information; and blood tests to analyze the types of circulating lipids and white blood cells. An independent validation group of 91 MS patients from the National Institute of Health with the same characteristics and additional control cohorts of healthy individuals within the same BMI range were similarly evaluated.
Researchers found that MS patients with high BMIs had higher ceramide levels and more circulating monocytes than were evident in healthy individuals with the same BMIs. High-BMI MS patients showed worsening disability and more brain lesions at the MRI compared to their normal BMI counterparts. The researchers went on to find that ceramides can enter inside immune cells called monocytes and change the way these cells read the genetic information encoded in the DNA. These epigenetic changes were also found in monocytes circulating in the blood of MS patients with high BMI.
Significance
The detection of ceramides inside the nucleus of blood cells and the ability of these lipids to induce epigenetic changes suggests that saturated fatty acids may have long-lasting functional effects, which over time steer the MS disease course towards worsening disability. In short, bad dietary habits may have negative consequences in healthy subjects, but they have an even more pronounced deleterious effect on patients with MS because the degrading myelin can accumulate and further increase ceramide levels.
“This study gives us a much-needed view into the environmental influences that can affect and change the behavior of cells in an individual’s body,” said Kamilah Castro, the paper’s first author and a graduate student in professor Casaccia’s lab. “Our findings suggest that increased levels of saturated fat as a result of dietary habits are one likely cause of the epigenetic changes that advance MS, which gives us a starting point for a potential intervention.”
The researchers’ findings support the concept of nutri-epigenomics (the ability of food to modify the way genomic information is interpreted by each cell) and the idea that lifestyle factors such as diet and weight can function as disease modifiers. Additional studies on larger cohorts are needed to validate the current findings. Further investigation is also needed to determine whether specific dietary interventions and weight management could be useful in helping MS patients manage and slow the progression of their disease and better respond to disease-modifying treatments.
“This translational study is exciting from a clinical perspective as it sheds light on a potentially important mechanism that can help explain our clinical observations regarding obesity and MS prognosis,” said Ilana Katz Sand, associate medical director of the Corinne Goldsmith Dickinson Center for MS at Mount Sinai. “We look forward to continuing to work on this important topic through future clinical studies to evaluate the impact of weight management and dietary intervention in MS.”
Source:
CUNY
Media Contacts:
Shawn Rhea – CUNY
Image Source:
The image is credited to Casaccia Lab.
Original Research: Open access.
“Body Mass Index in Multiple Sclerosis modulates ceramide-induced DNA methylation and disease course”
Castro, Kamilah et al. EBio Medicine, Volume 0, Issue 0, doi:10.1016/j.ebiom.2019.03.087
Abstract
Body Mass Index in Multiple Sclerosis modulates ceramide-induced DNA methylation and disease course
Background
Multiple Sclerosis (MS) results from genetic predisposition and environmental variables, including elevated Body Mass Index (BMI) in early life. This study addresses the effect of BMI on the epigenome of monocytes and disease course in MS.
Methods
Fifty-four therapy-naive Relapsing Remitting (RR) MS patients with high and normal BMI received clinical and MRI evaluation. Blood samples were immunophenotyped, and processed for unbiased plasma lipidomic profiling and genome-wide DNA methylation analysis of circulating monocytes. The main findings at baseline were validated in an independent cohort of 91 therapy-naïve RRMS patients. Disease course was evaluated by a two-year longitudinal follow up and mechanistic hypotheses tested in human cell cultures and in animal models of MS.
Findings
Higher monocytic counts and plasma ceramides, and hypermethylation of genes involved in negative regulation of cell proliferation were detected in the high BMI group of MS patients compared to normal BMI. Ceramide treatment of monocytic cell cultures increased proliferation in a dose-dependent manner and was prevented by DNA methylation inhibitors. The high BMI group of MS patients showed a negative correlation between monocytic counts and brain volume. Those subjects at a two-year follow-up showed increased T1 lesion load, increased disease activity, and worsened clinical disability. Lastly, the relationship between body weight, monocytic infiltration, DNA methylation and disease course was validated in mouse models of MS.
Interpretation
High BMI negatively impacts disease course in Multiple Sclerosis by modulating monocyte cell number through ceramide-induced DNA methylation of anti-proliferative genes.
Fund
This work was supported by funds from the Friedman Brain Institute, NIH, and Multiple Sclerosis Society.






