Summary: The side effects of administering ketamine to treat major depressive disorder are mild and persist for no longer than four hours, researchers report. Most of the side effects peaked within an hour of treatment, and many patients reported the effects as being significantly reduced two hours post ketamine administration.
Source: NIH/NIMH
National Institutes of Health researchers found that a single, low-dose ketamine infusion was relatively free of side effects for patients with treatment-resistant depression. Elia Acevedo-Diaz, M.D., Carlos Zarate, M.D., and colleagues at the NIH’s National Institute of Mental Health (NIMH) report their findings in the Journal of Affective Disorders.
Studies have shown that a single, subanesthetic-dose (a lower dose than would cause anesthesia) ketamine infusion can often rapidly relieve depressive symptoms within hours in people who have not responded to conventional antidepressants, which typically take weeks or months to work. However, widespread off-label use of intravenous subanesthetic-dose ketamine for treatment-resistant depression has raised concerns about side effects, especially given its history as a drug of abuse.
“The most common short-term side effect was feeling strange or loopy,” said Acevedo-Diaz, of the Section on the Neurobiology and Treatment of Mood Disorders, part of the NIMH Intramural Research Program (IRP) in Bethesda, Maryland. “Most side effects peaked within an hour of ketamine administration and were gone within two hours. We did not see any serious, drug-related adverse events or increased ketamine cravings with a single-administration.”
The researchers compiled data on side effects from 163 patients with major depressive disorder or bipolar disorder and 25 healthy controls who participated in one of five placebo-controlled clinical trials conducted at the NIH Clinical Center over 13 years. While past studies have been based mostly on passive monitoring, the NIMH IRP assessment involved active and structured surveillance of emerging side effects in an inpatient setting and used both a standard rating scale and clinician interviews. In addition to dissociative (disconnected, unreal) symptoms, the NIMH IRP assessment examined other potential side effects – including headaches, dizziness, and sleepiness. The study did not address the side effects associated with repeated infusions or long-term use.
Out of 120 possible side effects evaluated, 34 were found to be significantly associated with the treatment. Eight occurred in at least half of the participants: feeling strange, weird, or bizarre; feeling spacey; feeling woozy/loopy; dissociation; floating; visual distortions; difficulty speaking; and numbness. None persisted for more than four hours. No drug-related serious adverse events, cravings, propensity for recreational use, or significant cognitive or memory deficits were seen during a three-month follow-up.
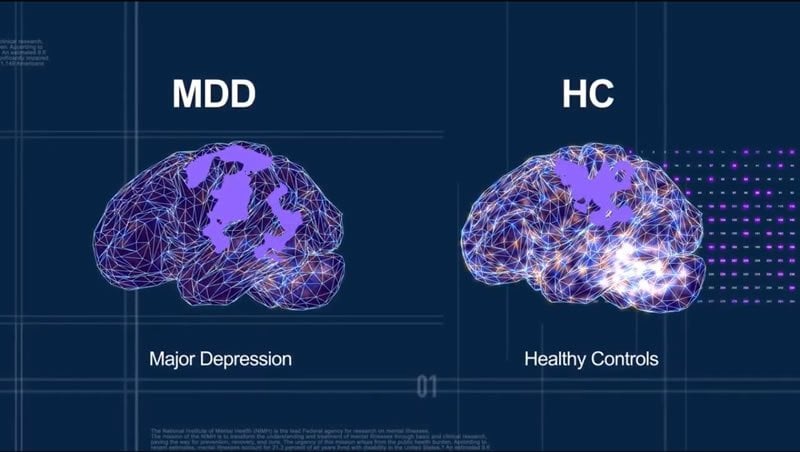
Credit: NIMH.
To overcome the limitations associated with side effects and intravenous delivery, ongoing research efforts seek to develop a more practical rapid-acting antidepressant that works in the brain similarly to ketamine. These NIMH researchers, in collaboration with the National Institute on Aging, and the National Center for Advancing Translational Science, are planning a clinical trial of a ketamine metabolite that showed promise as a potentially more specific-acting treatment in pre-clinical studies. Meanwhile, the U.S. Food and Drug Administration earlier this year approved an intranasal form of ketamine called esketamine, which can be administered to adults with treatment-resistant depression in a certified doctor’s office or clinic.
Source:
NIH/NIMH
Media Contacts:
Jules Asher – NIH/NIMH
Image Source:
The image is credited to NIMH.
Original Research: Closed access
“Comprehensive assessment of side effects associated with a single dose of ketamine in treatment-resistant depression.”. Acevedo-Diaz EE, Cavanaugh GW, Greenstein D, Kraus C, Kadriu B, Zarate CA Jr, Park LT.
Journal of Affective Disorders doi:10.1016/j.jad.2019.11.028.
Abstract
Comprehensive assessment of side effects associated with a single dose of ketamine in treatment-resistant depression.
Background
Concerns about ketamine for treating depression include abuse potential and the occurrence of psychotomimetic effects. This study sought to comprehensively assess side effects (SEs) associated with a single subanesthetic-dose intravenous ketamine infusion. A secondary aim was to examine the relationship between Clinician-Administered Dissociative States Scale (CADSS) scores and dissociative symptoms reported on a comprehensive, clinician-administered SE questionnaire.
Methods
Data from 188 participants were pooled from four placebo-controlled, crossover ketamine trials and one open-label study (n=163 with either treatment-resistant major depressive disorder or bipolar disorder and 25 healthy controls). SEs were actively solicited in a standardized fashion and monitored over the time-course of each study. Statistical analyses assessed the effect of drug (ketamine, placebo) on SEs and measured the relationship between CADSS total score and SEs contemporaneously endorsed during structured interviews.
Results
Forty-four of 120 SEs occurred in at least 5% of participants over all trials. Thirty-three of these 44 SEs were significantly associated with active drug administration (versus placebo). The most common SE was feeling strange/weird/loopy. Most SEs peaked within an hour of ketamine administration and resolved completely by two hours post-infusion. No serious drug-related adverse events or increased ketamine craving/abuse post-administration were observed. A positive correlation was found between dissociative SEs and total CADSS score.
Limitations
The post-hoc nature of the analysis; the limited generalizability of a single subanesthetic-dose ketamine infusion; and the lack of formal measures to assess ketamine’s cognitive, urological, or addictive potential.
Conclusions
No long-lasting significant SEs occurred over the approximately three-month follow-up period.






