Summary: People with a history of substance use disorder are more susceptible to COVID-19 infection and have an increased risk of experiencing worse outcomes, a new study reports.
Source: NIH/NIDA
A National Institutes of Health-funded study found that people with substance use disorders (SUDs) are more susceptible to COVID-19 and its complications. The research, published today in Molecular Psychiatry, was co-authored by Nora D. Volkow, M.D., director of the National Institute on Drug Abuse (NIDA). The findings suggest that health care providers should closely monitor patients with SUDs and develop action plans to help shield them from infection and severe outcomes.
By analyzing the non-identifiable electronic health records (EHR) of millions of patients in the United States, the team of investigators revealed that while individuals with an SUD constituted 10.3% of the total study population, they represented 15.6% of the COVID-19 cases. The analysis revealed that those with a recent SUD diagnosis on record were more likely than those without to develop COVID-19, an effect that was strongest for opioid use disorder, followed by tobacco use disorder. Individuals with an SUD diagnosis were also more likely to experience worse COVID-19 outcomes (hospitalization, death), than people without an SUD.
“The lungs and cardiovascular system are often compromised in people with SUD, which may partially explain their heightened susceptibility to COVID-19,” said Dr. Volkow. “Another contributing factor is the marginalization of people with addiction, which makes it harder for them to access health care services. It is incumbent upon clinicians to meet the unique challenges of caring for this vulnerable population, just as they would any other high-risk group.”
NIDA’s Dr. Volkow and Rong Xu, Ph.D., of Case Western Reserve University in Cleveland, Ohio, analyzed EHR data collected until June 15, 2020, from 360 hospitals nationwide. The EHRs were de-identified to ensure privacy.
The study population consisted of over 73 million patients, of which over 7.5 million had been diagnosed with an SUD at some point in their lives. Slightly more than 12,000 were diagnosed with COVID-19, and about 1,880 had both an SUD and a COVID-19 diagnosis on record. The types of SUDs investigated in the study were tobacco, alcohol, opioid, cannabis, and cocaine.
The complicating effects of SUD were visible in increased adverse consequences of COVID-19. Hospitalizations and death rates of COVID-19 patients were all elevated in people with recorded SUDs compared to those without (41.0% versus 30.1% and 9.6% versus 6.6%, respectively).
Additionally, African Americans with a recent opioid use disorder diagnosis were over four times more likely to develop COVID-19, compared to whites. Results showed that hypertension, diabetes, cardiovascular diseases, and renal diseases, which are risk factors for COVID-19, were more prevalent among African Americans than whites with opioid use disorder.
According to the authors, the study findings underscore the need to screen for, and treat, SUDs as part of the strategy for controlling the pandemic. Additional research needs to be done to better understand how best to treat those with SUDs who are at risk for COVID-19 and counsel on how to avoid the risk of infection.
Funding: This research was funded by NIDA, the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Institute on Aging, all parts of NIH, as well as the American Cancer Society and The Clinical and Translational Science Collaborative of Cleveland.
About this migraine research article
Source:
NIH/NIDA
Contacts:
NIDA Press Office – NIH/NIDA
Image Source:
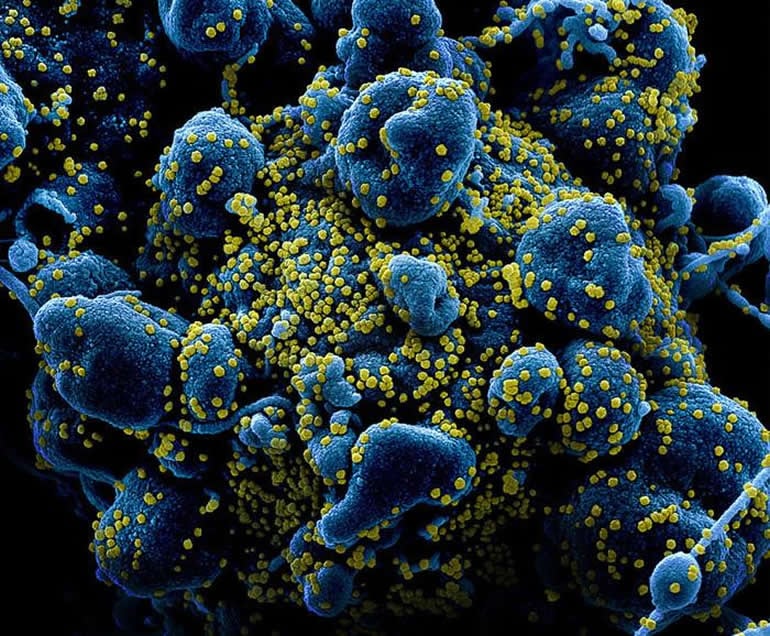
The image is credited to NIAID.
Original Research: Open access
“COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States” by Wang Q, Kaelber D, Xu R, Volkow ND. Molecular Psychiatry.
Abstract
COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United Statesl
The global pandemic of COVID-19 is colliding with the epidemic of opioid use disorders (OUD) and other substance use disorders (SUD) in the United States (US). Currently, there is limited data on risks, disparity, and outcomes for COVID-19 in individuals suffering from SUD. This is a retrospective case-control study of electronic health records (EHRs) data of 73,099,850 unique patients, of whom 12,030 had a diagnosis of COVID-19. Patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 8.699 [8.411–8.997], P < 10−30), an effect that was strongest for individuals with OUD (AOR = 10.244 [9.107–11.524], P < 10−30), followed by individuals with tobacco use disorder (TUD) (AOR = 8.222 ([7.925–8.530], P < 10−30). Compared to patients without SUD, patients with SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer. Among patients with recent diagnosis of SUD, African Americans had significantly higher risk of COVID-19 than Caucasians (AOR = 2.173 [2.01–2.349], P < 10−30), with strongest effect for OUD (AOR = 4.162 [3.13–5.533], P < 10−25). COVID-19 patients with SUD had significantly worse outcomes (death: 9.6%, hospitalization: 41.0%) than general COVID-19 patients (death: 6.6%, hospitalization: 30.1%) and African Americans with COVID-19 and SUD had worse outcomes (death: 13.0%, hospitalization: 50.7%) than Caucasians (death: 8.6%, hospitalization: 35.2%). These findings identify individuals with SUD, especially individuals with OUD and African Americans, as having increased risk for COVID-19 and its adverse outcomes, highlighting the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support.






