New research reveals traumatic brain injury patients struggle with discipline in social, family and work life
New research finds people with traumatic brain injuries (TBI) –such as those incurred from violent accidents or combat — are more prone to misjudge when faced with situations involving dispute or requiring discipline.
The study, led in part by Dr. Jordan Grafman at the Rehabilitation Institute of Chicago and published this month in Social Cognitive and Affective Neuroscience (SCAN), is the first to objectively assess how people with frontal lobe lesions punish — a key indicator for how they will function in society. These findings can guide doctors in providing patients with more effective treatment.
Traumatic brain injury is pervasive in America, affecting nearly 2 million patients per year, as well as countless others, including family members, colleagues and people encountered in everyday activities.
TBI is often connected to altered social behaviors — from the veteran struggling with a short temper to the football player in hot water for public altercations. This new research sheds additional light on this connection by focusing on a common effect of TBI, frontal lobe injuries, and how these injuries affect a patient’s ability to punish.
“The ability to judge such things as a business dispute, family argument or a child’s misbehavior and then assess reasonable discipline is fairly indicative of one’s ability to rationally and socially integrate within society,” said Grafman, Ph.D., study investigator and director of brain injury research at the Rehabilitation Institute of Chicago. “This study finds that those suffering from penetrating TBI may not have the capacity to appropriately assess proper punishments, a factor which suggests how people will do in the real world.”
Impartial third-party punishment, or TPP, is the ability to judge the severity of a crime and assess a reasonable punishment. If a patient struggles with TPP, he or she likely struggles with several important social skills, such as interpreting another person’s intentions, showing empathy and making rational judgments. The absence of these skills, which regulate behavior, indicate poorer prognoses for resuming normal work, school and family life.
From 2009 to 2012, Dr. Grafman’s team worked with 114 Vietnam War veterans who had suffered penetrating brain injuries as part of the ongoing Vietnam Head Injury Study, an investigation launched in 1967 and sponsored by various entities, including the Department of Defense and the National Institutes of Health. The study includes more than 100 research projects, and Dr. Grafman has been lead investigator for the Vietnam War-related projects since 1990.
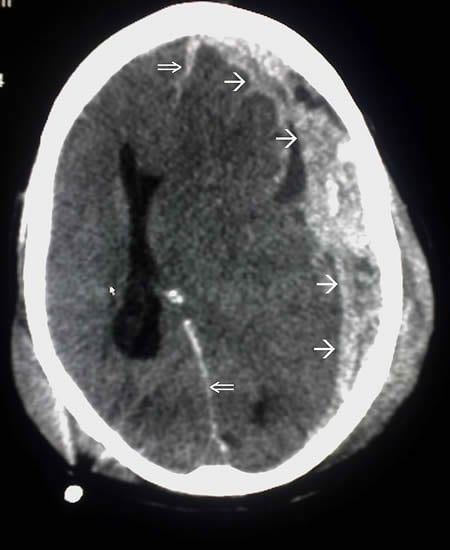
In this study, researchers used whole-brain imaging to pinpoint damage in the subjects’ brains. They also gave the subjects a series of tests to measure various abilities, including the ability to put items in order, remember things or judge the severity of a crime.
To test the ability to judge severity, they showed each subject index cards describing 24 different scenarios, ranging from innocuous activities such as delaying an oil change to graphic violence. The veterans rank-ordered the cards to reflect the relative degree of punishment deserved.
The researchers repeated the experiment with 32 non-injured Vietnam-era combat veterans, who served as a control group.
Study findings underscored the significance of frontal lobe injuries. Veterans with frontal lobe injuries did worse than the control group when it came to assigning inappropriate punishments, and pinpointed for researchers the brain locations of the underlying problems. For example, subjects with altruism deficits tended to have right frontal lobe injuries, while subjects who had trouble forming concepts (the ability to determine the overall theme from different pieces of information) showed left lobe damage.
“This is a translational study with important implications for clinical and real-world settings,” said Grafman. “Having deeper understanding of challenges faced by patients with frontal lobe injuries — whether due to a traumatic brain injury, stroke, tumor or other neurological disorder — can guide doctors in providing patients with more effective treatment. The goal is always to find new and better ways to help patients recovering from traumatic brain injuries — and their families — at home, at work and in society.”
In addition to Grafman, the study was authored by Leila Glass, Frank Krueger and Lara Moody.
Funding: The work was supported by Department of Defense, National Institutes of Health.
Source: Megan Washburn – Rehabilitation Institute of Chicago
Image Credit: The image is in the public domain
Original Research: Abstract for “Neural signatures of third-party punishment: evidence from penetrating traumatic brain injury” by Leila Glass, Lara Moody, Jordan Grafman, and Frank Krueger in Social Cognitive and Affective Neuroscience. Published online August 13 2015 doi:10.1093/scan/nsv105
Abstract
Neural signatures of third-party punishment: evidence from penetrating traumatic brain injury
The ability to survive within a cooperative society depends on impartial third-party punishment (TPP) of social norm violations. Two cognitive mechanisms have been postulated as necessary for the successful completion of TPP: evaluation of legal responsibility and selection of a suitable punishment given the magnitude of the crime. Converging neuroimaging research suggests two supporting domain-general networks; a mentalizing network for evaluation of legal responsibility and a central-executive network for determination of punishment. A whole-brain voxel-based lesion-symptom mapping approach was used in conjunction with a rank-order TPP task to identify brain regions necessary for TPP in a large sample of patients with penetrating traumatic brain injury. Patients who demonstrated atypical TPP had specific lesions in core regions of the mentalizing (dorsomedial prefrontal cortex [PFC], ventromedial PFC) and central-executive (bilateral dorsolateral PFC, right intraparietal sulcus) networks. Altruism and executive functioning (concept formation skills) were significant predictors of TPP: altruism was uniquely associated with TPP in patients with lesions in right dorsolateral PFC and executive functioning was uniquely associated with TPP in individuals with lesions in left PFC. Our findings contribute to the extant literature to support underlying neural networks associated with TPP, with specific brain-behavior causal relationships confirming recent functional neuroimaging research.
“Neural signatures of third-party punishment: evidence from penetrating traumatic brain injury” by Leila Glass, Lara Moody, Jordan Grafman, and Frank Krueger in Social Cognitive and Affective Neuroscience. Published online August 13 2015 doi:10.1093/scan/nsv105






