Summary: According to a new study, rats with hypopituitarism received pituitary cell transplants, which promoted normal hormone release.
Source: Cell Press.
Researchers have successfully used human stem cells to generate functional pituitary tissue that secretes hormones important for the body’s stress response as well as for its growth and reproductive functions. When transplanted into rats with hypopituitarism, a disease linked to dwarfism and premature aging in humans, the lab-grown pituitary cells promoted normal hormone release. The study, which lays the foundation for future preclinical work, appears June 14 in Stem Cell Reports.
“The current treatment options for patients suffering from hypopituitarism, a dysfunction of the pituitary gland, are far from optimal,” says first study author Bastian Zimmer of the Sloan Kettering Institute for Cancer Research. “Cell replacement could offer a more permanent therapeutic option with pluripotent stem cell-derived hormone-producing cells that functionally integrate and respond to positive and negative feedback from the body. Achieving such a long-term goal may lead to a potential cure, not only a treatment, for those patients.”
The pituitary gland is the master regulator of hormone production in the body, releasing hormones that play a key role in bone and tissue growth, metabolism, reproductive functions, and the stress response. Hypopituitarism can be caused by tumors, genetic defects, brain trauma, immune and infectious diseases, or radiation therapy. The consequences of pituitary dysfunction are wide ranging and particularly serious in children, who can suffer severe learning disabilities, growth and skeletal problems, as well as effects on puberty and sexual function.
Currently, patients with hypopituitarism must take expensive, lifelong hormone replacement therapies that poorly mimic the body’s complex patterns of hormone secretion that fluctuates with circadian rhythms and responds to feedback from other organs. By contrast, cell replacement therapies hold promise for permanently restoring natural patterns of hormone secretion while avoiding the need for costly, lifelong treatments.
Recently, scientists developed a procedure for generating pituitary cells from human pluripotent stem cells–an unlimited cell source for regenerative medicine–using organoid cultures that mimic the 3D organization of the developing pituitary gland. However, this approach is inefficient and complicated, relies on ill-defined cellular signals, lacks reproducibility, and is not scalable or suitable for clinical-grade cell manufacturing.
To address these limitations, Zimmer and senior study author Lorenz Studer of the Sloan Kettering Institute for Cancer Research developed a simple, efficient, and robust stem cell-based strategy for reliably producing a large number of diverse, functional pituitary cell types suitable for therapeutic use. Instead of mimicking the complex 3D organization of the developing pituitary gland, this approach relies on the precisely timed exposure of human pluripotent stem cells to a few specific cellular signals that are known to play an important role during embryonic development.
Exposure to these proteins triggered the stem cells to turn into different types of functional pituitary cells that released hormones important for bone and tissue growth (i.e., growth hormone), the stress response (i.e., adrenocorticotropic hormone), and reproductive functions (i.e., prolactin, follicle-stimulating hormone, and luteinizing hormone). Moreover, these stem cell-derived cells released different amounts of hormone in response to known feedback signals generated by other organs in the body.
To test the therapeutic potential of this approach, the researchers transplanted the stem cell-derived pituitary cells under the skin of rats whose pituitary gland had been surgical removed. The cell grafts not only secreted adrenocorticotropic hormone, prolactin, and follicle-stimulating hormone, but they also triggered appropriate hormonal responses in the kidneys.
The researchers were also able to control the relative composition of different hormonal cell types simply by exposing human pluripotent stem cells to different ratios of two proteins: fibroblast growth factor 8 and bone morphogenetic protein 2. This finding suggests their approach could be tailored to generate specific cell types for patients with different types of hypopituitarism. “For the broad application of stem cell-derived pituitary cells in the future, cell replacement therapy may need to be customized to the specific needs of a given patient population,” Zimmer says.
In future studies, the researchers plan to further improve the protocol to generate pure populations of various hormone-releasing cell types, enabling the production of grafts that are tailored to the needs of individual patients. They will also test this approach on more clinically relevant animal models that have pituitary damage caused by radiation therapy and receive grafts in or near the pituitary gland rather than under the skin. This research could have important implications for cancer survivors, given that hypopituitarism is one of the main causes of poor quality of life after brain radiation therapy.
“Our findings represent a first step in treating hypopituitarism, but that does not mean the disease will be cured permanently within the near future,” Zimmer says. “However, our work illustrates the promise of human pluripotent stem cells as it presents a direct path toward realizing the promise of regenerative medicine for certain hormonal disorders.”
Funding: The researchers were supported by the New York State Stem Cell Science and the Starr Foundation. The work was further supported in part by the National Institutes of Health and the National Cancer Institute.
Source: Joseph Caputo – Cell Press
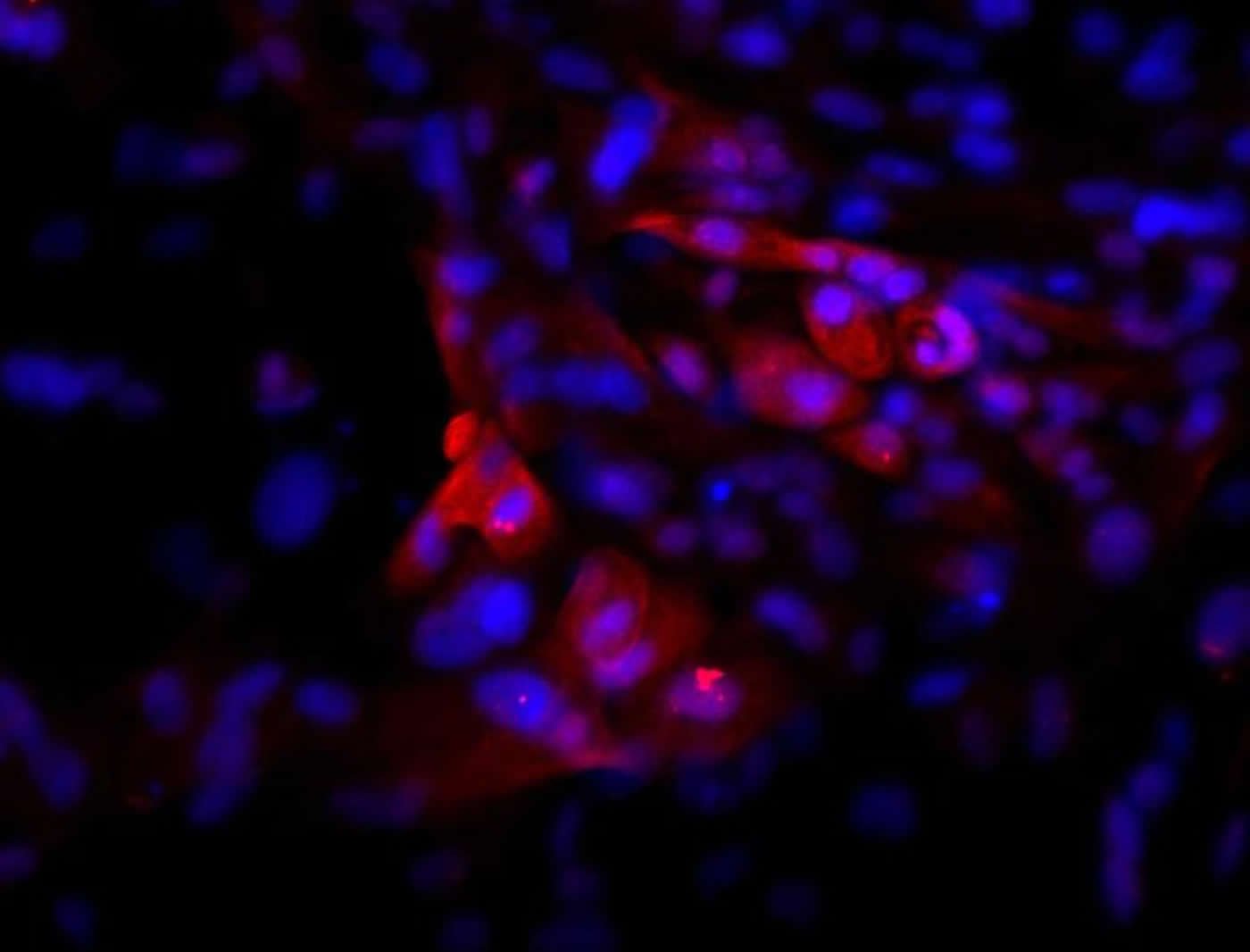
Image Source: This NeuroscienceNews.com image is credited to Bastian Zimmer, Sloan Kettering Institute.
Original Research: Full open access research for “Derivation of Diverse Hormone-Releasing Pituitary Cells from Human Pluripotent Stem Cells” by Bastian Zimmer, Jinghua Piao, Kiran Ramnarine, Mark J. Tomishima, Viviane Tabar, and Lorenz Studer in Stem Cell Reports. Published online June 14 2016 doi:10.1016/j.stemcr.2016.05.005
[cbtabs][cbtab title=”MLA”]Cell Press. “Pituitary Tissue Grown From Human Stem Cells Releases Hormones in Rats.” NeuroscienceNews. NeuroscienceNews, 14 June 2016.
<https://neurosciencenews.com/stem-cell-transplant-hormones-4463/>.[/cbtab][cbtab title=”APA”]Cell Press. (2016, June 14). Pituitary Tissue Grown From Human Stem Cells Releases Hormones in Rats. NeuroscienceNews. Retrieved June 14, 2016 from https://neurosciencenews.com/stem-cell-transplant-hormones-4463/[/cbtab][cbtab title=”Chicago”]Cell Press. “Pituitary Tissue Grown From Human Stem Cells Releases Hormones in Rats.” https://neurosciencenews.com/stem-cell-transplant-hormones-4463/ (accessed June 14, 2016).[/cbtab][/cbtabs]
Abstract
Derivation of Diverse Hormone-Releasing Pituitary Cells from Human Pluripotent Stem Cells
Highlights
•Defined, cGMP-ready protocol to derive anterior pituitary-lineage cells from hPSCs
•FGF8 and BMP2 patterning enables enrichment for specific hormone-producing cells
•Pituitary cells secrete multiple hormones and respond to physiological stimuli
•hPSC-pituitary cells partially rescue a rat model of hypopituitarism
Summary
Human pluripotent stem cells (hPSCs) provide an unlimited cell source for regenerative medicine. Hormone-producing cells are particularly suitable for cell therapy, and hypopituitarism, a defect in pituitary gland function, represents a promising therapeutic target. Previous studies have derived pituitary lineages from mouse and human ESCs using 3D organoid cultures that mimic the complex events underlying pituitary gland development in vivo. Instead of relying on unknown cellular signals, we present a simple and efficient strategy to derive human pituitary lineages from hPSCs using monolayer culture conditions suitable for cell manufacturing. We demonstrate that purified placode cells can be directed into pituitary fates using defined signals. hPSC-derived pituitary cells show basal and stimulus-induced hormone release in vitro and engraftment and hormone release in vivo after transplantation into a murine model of hypopituitarism. This work lays the foundation for future cell therapy applications in patients with hypopituitarism.
“Derivation of Diverse Hormone-Releasing Pituitary Cells from Human Pluripotent Stem Cells” by Bastian Zimmer, Jinghua Piao, Kiran Ramnarine, Mark J. Tomishima, Viviane Tabar, and Lorenz Studer in Stem Cell Reports. Published online June 14 2016 doi:10.1016/j.stemcr.2016.05.005






