A commonly prescribed antidepressant may alter brain structures in depressed and non-depressed individuals in very different ways, according to new research at Wake Forest Baptist Medical Center.
The study – conducted in nonhuman primates with brain structures and functions similar to those of humans – found that the antidepressant sertraline, a selective serotonin reuptake inhibitor (SSRI) marketed as Zoloft, significantly increased the volume of one brain region in depressed subjects but decreased the volume of two brain areas in non-depressed subjects.
“These observations are important for human health because Zoloft is widely prescribed for a number of disorders other than depression,” said Carol A. Shively, Ph.D., professor of pathology-comparative medicine at Wake Forest Baptist and lead author of the study, published in the current online issue of the journal Neuropharmacology.
In the study, 41 middle-aged female monkeys were fed a diet formulated to replicate that consumed by many Americans for 18 months, during which time depressive behavior in the animals was recorded. Female monkeys were chosen for this study because depression is nearly twice as common in women as men and the use of antidepressants is most common in women ages 40 to 59.
After the 18-month pre-study phase, the monkeys were divided into two groups balanced for body weight, body mass index and depressive behavior. For the next 18 months, 21 monkeys received sertraline in daily doses comparable to those taken by humans while a group of 20 received a placebo. This treatment regimen is analogous to a human taking an antidepressant for approximately five years.
MRI images taken at the end of the treatment phase revealed that in depressed subjects the drug significantly increased the volume of one region of the brain, the anterior cingulate cortex, while decreasing the volume of this same region and the hippocampus in non-depressed subjects. Both of these areas are highly interconnected with other areas of the brain; are critical in a wide array of functions including memory, learning, spatial navigation, will, motivation and emotion; and are implicated in major depressive disorder.
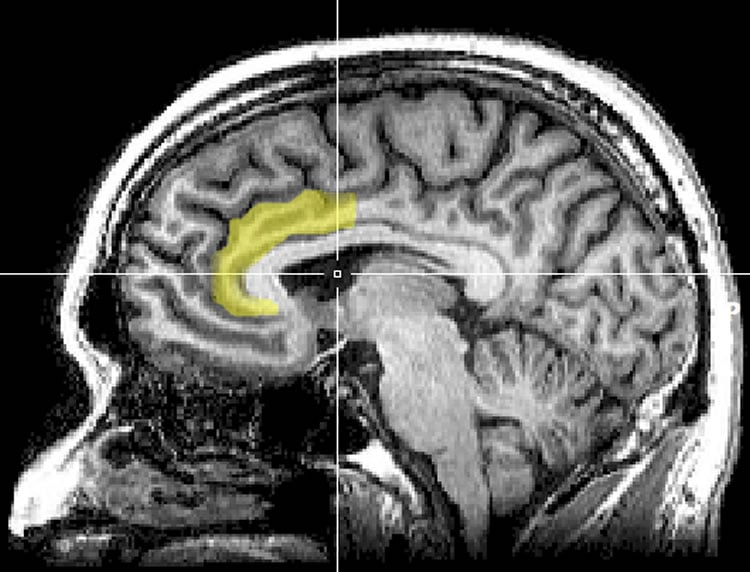
In humans, Shively said, volume differences in neural structures have been noted in depressed and non-depressed individuals, with the most commonly reported differences being smaller volumes of the cingulate cortex and hippocampus in depressed people. One potential mechanism through which drugs such as Zoloft can be effective as antidepressants is by promoting neuron growth and connectivity in these brain regions.
But SSRIs, including Zoloft, are prescribed for a variety of disorders besides depression, including bulimia, hot flashes, obsessive-compulsive disorder, post-traumatic stress disorder, stroke recovery and sexual dysfunction, and there are no studies of the effects of these drugs on brain volumes in individuals not diagnosed with depression.
“The study’s findings regarding the different effects of sertraline on brain-region volumes in depressed versus non-depressed subjects are compelling,” Shively said. “But given the number of different disorders for which SSRIs are prescribed, the findings need to be investigated further in patient populations to see if these drugs produce similar effects in humans.”
Co-authors of the study are J. Daniel Bourland, Ph.D., Ashlee Clark, M.S., James B. Daunais, Ph.D., Warwick D. Johnston, B.A., Sara R. Jones, Ph.D., Robert A. Kraft, Ph.D., Adreanna Massey, B.A., David Neely, B.S., Beth Uberseder, B.S., and Jeff D. Williamson, M.D., of Wake Forest Baptist and Stephanie L. Willard, Ph.D., of the University of Pennsylvania.
Funding: The study was funded in part by National Institutes of Health grant HL078103.
Source: Marguerite Beck – Wake Forest Baptist Medical Center
Image Source: The image is credited to Geoff B Hall and is in the public domain
Original Research: Abstract for “Long term sertraline effects on neural structures in depressed and nondepressed adult female nonhuman primates” by Stephanie L. Willard, Beth Uberseder, Ashlee Clark, James B. Daunais, Warwick D. Johnston, David Neely, Adreanna Massey, Jeff D. Williamson, Robert A. Kraft, J. Daniel Bourland, Sara R. Jones, and Carol A. Shivelyin Neuropharmacology. Published online June 24 2015 doi:10.1016/j.neuropharm.2015.06.011
Abstract
Long term sertraline effects on neural structures in depressed and nondepressed adult female nonhuman primates
Background
Selective serotonin reuptake inhibitors (SSRIs) are widely prescribed for mood and other disorders. However, their neural effects are difficult to study due to patient compliance and drug history variability, and rarely studied in those prescribed SSRIs for non-mood disorders. Here we evaluated SSRI effects on neural volumetrics in depressed and nondepressed monkeys.
Methods
42 socially-housed cynomolgus monkeys were randomized to treatment balanced on pretreatment depressive behavior and body weight. Monkeys were trained for oral administration of placebo or 20 mg/kg sertraline HCl daily for 18 months and depressive and anxious behavior recorded. Volumes of neural regions of interest in depression were measured in magnetic resonance images and analyzed by 2 (depressed, nondepressed) × 2 (placebo, sertraline) ANOVA.
Results
Sertraline reduced anxiety (p = 0.04) but not depressive behavior (p = 0.43). Left Brodmann’s Area (BA) 32 was smaller in depressed than nondepressed monkeys (main effect of depression: p < 0.05). Sertraline and depression status interacted to affect volumes of left Anterior Cingulate Cortex (ACC), left BA24, right hippocampus (HC), and right anterior HC (sertraline × depression interactions: all p's < 0.05). In the Placebo group, depressed monkeys had smaller right anterior HC and left ACC than nondepressed monkeys. In nondepressed monkeys, sertraline reduced right HC volume, especially right anterior HC volume. In depressed monkeys sertraline increased left ACC volume. In nondepressed monkeys, sertraline reduced left BA24 volumes resulting in smaller BA24 volumes in nondepressed than sertraline-treated depressed monkeys. Conclusions
These observations suggest that SSRIs may differentially affect neural structures in depressed and nondepressed individuals.
“Long term sertraline effects on neural structures in depressed and nondepressed adult female nonhuman primates” by Stephanie L. Willard, Beth Uberseder, Ashlee Clark, James B. Daunais, Warwick D. Johnston, David Neely, Adreanna Massey, Jeff D. Williamson, Robert A. Kraft, J. Daniel Bourland, Sara R. Jones, and Carol A. Shivelyin Neuropharmacology. Published online June 24 2015 doi:10.1016/j.neuropharm.2015.06.011






