Findings add urgency to screening and treatment.
The AIDS virus can genetically evolve and independently replicate in patients’ brains early in the illness process, researchers funded by the National Institutes of Health have discovered. An analysis of cerebral spinal fluid (CSF), a window into brain chemical activity, revealed that for a subset of patients HIV had started replicating within the brain within the first four months of infection. CSF in 30 percent of HIV-infected patients tracked showed at least transient signs of inflammation – suggesting an active infectious process – or viral replication within the first two years of infection. There was also evidence that the mutating virus can evolve a genome in the central nervous system that is distinct from that in the periphery.
“These results underscore the importance of early diagnosis and treatment with antiretroviral therapy,” said Dianne Rausch, Ph.D., director of the Division of AIDS Research of the NIH’s National Institute of Mental Health (NIMH). “Any delay runs the risk that the virus could find refuge and cause damage in the brain, where some medications are less effective – potentially enabling it to re-emerge, even after it is suppressed in the periphery.”
NIMH grantees Serena Spudich, M.D., of Yale University, New Haven, Connecticut; Ronald Swanstrom, Ph.D., of the University of North Carolina, Chapel Hill; Richard Price, M.D., University of California, San Francisco; and Christa Buckheit Sturdevant, Ph.D., UNC (now at Duke), and colleagues, report on their findings March 26, 2015, in the journal PLoS Pathogens.
Prior to the study, it was known that HIV readily penetrates the brain and can trigger neurological problems and eventually cause dementia over the course of the infection. Yet there was little evidence about how quickly it can take hold and thrive there. Nor was it clear to what extent the brain serves as a hard-to-reach hideout from which the virus might re-infect the body – even if it is eliminated from peripheral blood and lymph node tissue by treatment.
To learn more, the researchers compared evidence of HIV activity in CSF versus blood from 72 untreated HIV-infected patients over the first two years of their infection. Overall, 10-22 percent of the patients showed evidence of HIV replication or inflammation in the brain at the different time points analyzed within the first two years – and the signs persisted over time in about 16 percent of the participants.
The evidence suggests that in most patients peripheral forms of the virus infect immune cells that spread to the brain via blood. Yet in some patients, genetic versions of the virus not found in blood evolve in the brain environment. So it could become an independent, compartmentalized viral reservoir, capable of generating treatment-resistant mutant forms that could break out and re-infect the rest of the body after seemingly successful treatment, explained Rausch.
Whether the potential brain damage caused by early HIV replication and inflammation might be reversible with antiviral therapy awaits further research, said Swanstrom.
The research was funded by NIH/National Institute of Mental Health.
Grants: MH099979, MH101024, MH094177, MH074466
Contact: Jules Asher – NIH/NIMH
Source: NIH/NIMH press release
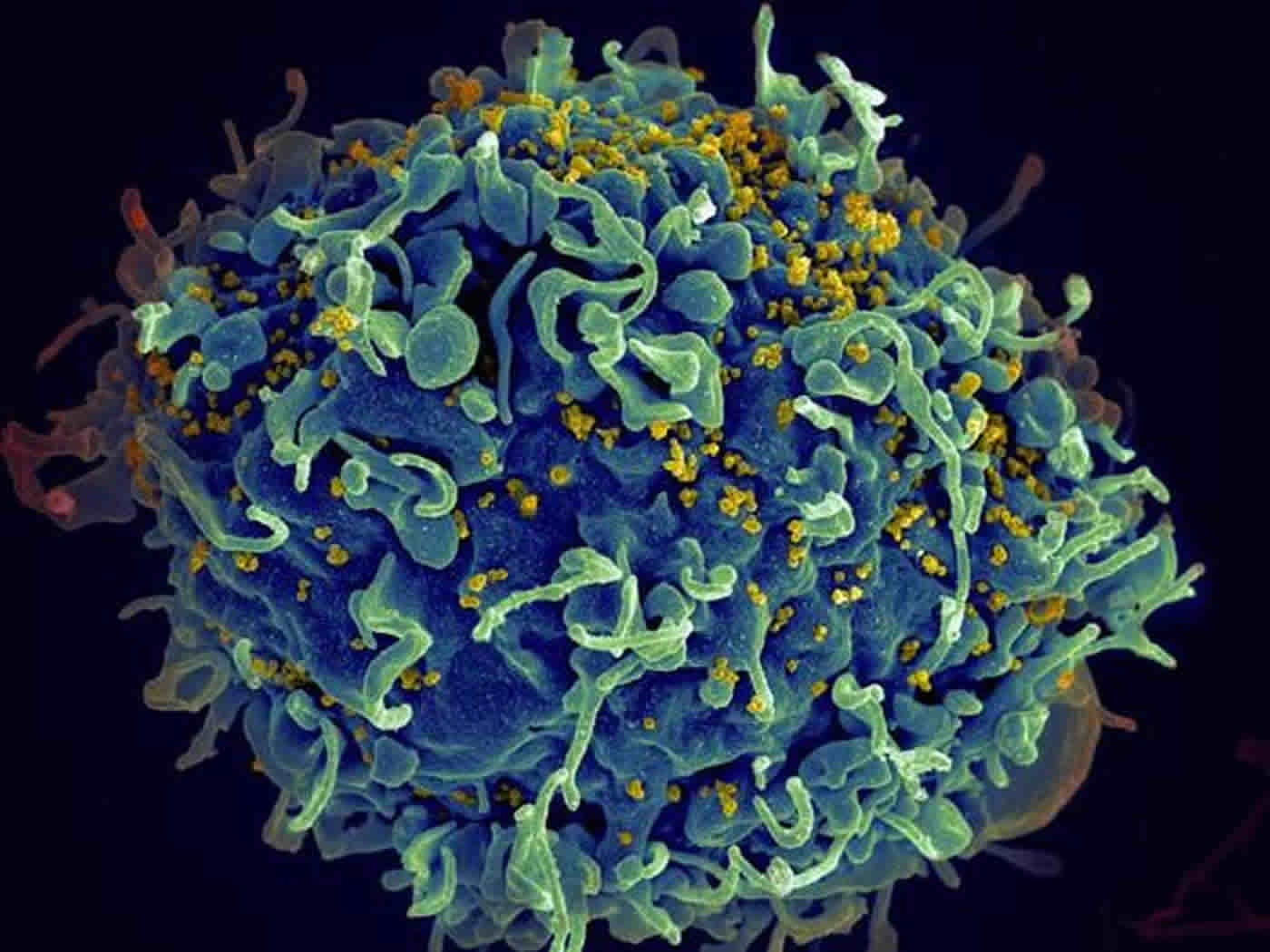
Image Source: The image is credited to Seth Pincus, Elizabeth Fischer and Austin Athman, National Institute of Allergy and Infectious Diseases, National Institutes of Health and is adapted from the NIH/NIMH press release
Original Research: Full open access research for “Compartmentalized replication of R5 T Cell-Tropic HIV-1 in the central nervous system early in the course of infection” by Christa Buckheit Sturdevant, Sarah B. Joseph, Gretja Schnell, Richard W. Price, Ronald Swanstrom, and Serena Spudich in PLOS Pathogens. Published online March 26 2015 doi:10.1371/journal.ppat.1004720
Compartmentalized Replication of R5 T Cell-Tropic HIV-1 in the Central Nervous System Early in the Course of Infection
Compartmentalized HIV-1 replication within the central nervous system (CNS) likely provides a foundation for neurocognitive impairment and a potentially important tissue reservoir. The timing of emergence and character of this local CNS replication has not been defined in a population of subjects. We examined the frequency of elevated cerebrospinal fluid (CSF) HIV-1 RNA concentration, the nature of CSF viral populations compared to the blood, and the presence of a cellular inflammatory response (with the potential to bring infected cells into the CNS) using paired CSF and blood samples obtained over the first two years of infection from 72 ART-naïve subjects. Using single genome amplification (SGA) and phylodynamics analysis of full-length env sequences, we compared CSF and blood viral populations in 33 of the 72 subjects. Independent HIV-1 replication in the CNS (compartmentalization) was detected in 20% of sample pairs analyzed by SGA, or 7% of all sample pairs, and was exclusively observed after four months of infection. In subjects with longitudinal sampling, 30% showed evidence of CNS viral replication or pleocytosis/inflammation in at least one time point, and in approximately 16% of subjects we observed evolving CSF/CNS compartmentalized viral replication and/or a marked CSF inflammatory response at multiple time points suggesting an ongoing or recurrent impact of the infection in the CNS. Two subjects had one of two transmitted lineages (or their recombinant) largely sequestered within the CNS shortly after transmission, indicating an additional mechanism for establishing early CNS replication. Transmitted variants were R5 T cell-tropic. Overall, examination of the relationships between CSF viral populations, blood and CSF HIV-1 RNA concentrations, and inflammatory responses suggested four distinct states of viral population dynamics, with associated mechanisms of local viral replication and the early influx of virus into the CNS. This study considerably enhances the generalizability of our results and greatly expands our knowledge of the early interactions of HIV-1 in the CNS.
“Compartmentalized replication of R5 T Cell-Tropic HIV-1 in the central nervous system early in the course of infection” by Christa Buckheit Sturdevant, Sarah B. Joseph, Gretja Schnell, Richard W. Price, Ronald Swanstrom, and Serena Spudich in PLOS Pathogens doi:10.1371/journal.ppat.1004720






