Summary: New research could help develop treatments for secondary progressive multiple sclerosis.
Source: Brigham and Women’s Hospital.
Study sheds light on the biology of progressive form of multiple sclerosis, suggests a new potential path for treatment.
A research team led by scientists from Brigham and Women’s Hospital has revealed how an FDA-approved drug works in the central nervous system in mice to suppress chronic inflammation. The drug, known as FTY720 (or Fingolimod) interferes with signals sent through sphingosine-1-phosphate receptors, and appears to reduce the pathogenic activities of astrocytes. The findings suggest the treatment may hold promise for a progressive and difficult-to-treat form of multiple sclerosis (MS) known as secondary progressive MS (SPMS).
“One of the most important unmet clinical needs in MS is to design therapeutic approaches for the progressive phase of the disease,” said senior author Francisco Quintana, PhD, a researcher in the Ann Romney Center for Neurologic Diseases at BWH. “And a key unanswered question related to that is, what are the biological processes that drive disease pathogenesis at this stage?”
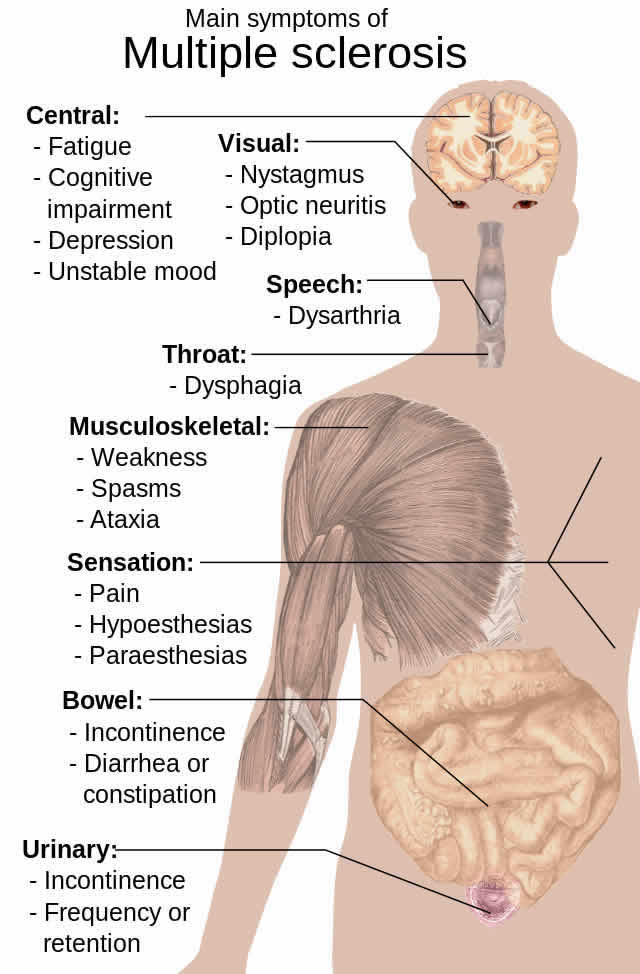
MS is a chronic autoimmune disease that affects the central nervous system. It frequently begins with a relapsing-remitting course that often gives way to second phase, SPMS, which is characterized by severe and irreversible neurological decline. Unfortunately, there are few therapies that target this form of MS. Notably, treatments for the relapsing-remitting phase of the disease are ineffective against SPMS.
The current study, published in PNAS and led by Quintana and his colleagues, sheds new light on the role of sphingosine-1-phosphate, a type of lipid, and its receptors in SPMS. The researchers found that blockage of these signals with FTY720 had important effects on astrocytes in both mice and humans, decreasing their pro-inflammatory and neurotoxic properties while also increasing the cells’ anti-inflammatory capabilities.
Although the findings are noteworthy, the neuroprotective effects Quintana and his colleagues observe are not as strong as those they have recorded in previous studies of other drugs. Nevertheless, the results suggest FTY720 may help mitigate some aspects of SPMS in humans. A clinical trial of a highly related drug, led by Novartis, is now underway and encouraging preliminary results have been recently released, Quintana said.
Source: Lori Schroth – Brigham and Women’s Hospital
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “Sphingosine-1-phosphate receptor modulation suppresses pathogenic astrocyte activation and chronic progression CNS inflammation” by Veit Rothhammer, Jessica E. Kenison, Emily Tjon, Maisa C. Takenaka, Kalil Alves de Lima, Davis M. Borucki, Chun-Cheih Chao, Annabel Wilz, Manon Blain, Luke Healy, Jack Antel, and Francisco J. Quintana in PNAS. Published online February 6 2017 doi:10.1073/pnas.1615413114
[cbtabs][cbtab title=”MLA”]Brigham and Women’s Hospital “Shedding Light on the Biology of Progressive Form of Multiple Sclerosis.” NeuroscienceNews. NeuroscienceNews, 8 February 2017.
<https://neurosciencenews.com/progressive-ms-neurobiology-6085/>.[/cbtab][cbtab title=”APA”]Brigham and Women’s Hospital (2017, February 8). Shedding Light on the Biology of Progressive Form of Multiple Sclerosis. NeuroscienceNew. Retrieved February 8, 2017 from https://neurosciencenews.com/progressive-ms-neurobiology-6085/[/cbtab][cbtab title=”Chicago”]Brigham and Women’s Hospital “Shedding Light on the Biology of Progressive Form of Multiple Sclerosis.” https://neurosciencenews.com/progressive-ms-neurobiology-6085/ (accessed February 8, 2017).[/cbtab][/cbtabs]
Abstract
Sphingosine-1-phosphate receptor modulation suppresses pathogenic astrocyte activation and chronic progression CNS inflammation
Multiple sclerosis (MS) is an autoimmune inflammatory demyelinating disease of the CNS that causes disability in young adults as a result of the irreversible accumulation of neurological deficits. Although there are potent disease-modifying agents for its initial relapsing-remitting phase, these therapies show limited efficacy in secondary progressive MS (SPMS). Thus, there is an unmet clinical need for the identification of disease mechanisms and potential therapeutic approaches for SPMS. Here, we show that the sphingosine 1-phosphate receptor (S1PR) modulator fingolimod (FTY720) ameliorated chronic progressive experimental autoimmune encephalomyelitis in nonobese diabetic mice, an experimental model that resembles several aspects of SPMS, including neurodegeneration and disease progression driven by the innate immune response in the CNS. Indeed, S1PR modulation by FTY720 in murine and human astrocytes suppressed neurodegeneration-promoting mechanisms mediated by astrocytes, microglia, and CNS-infiltrating proinflammatory monocytes. Genome-wide studies showed that FTY720 suppresses transcriptional programs associated with the promotion of disease progression by astrocytes. The study of the molecular mechanisms controlling these transcriptional modules may open new avenues for the development of therapeutic strategies for progressive MS.
“Sphingosine-1-phosphate receptor modulation suppresses pathogenic astrocyte activation and chronic progression CNS inflammation” by Veit Rothhammer, Jessica E. Kenison, Emily Tjon, Maisa C. Takenaka, Kalil Alves de Lima, Davis M. Borucki, Chun-Cheih Chao, Annabel Wilz, Manon Blain, Luke Healy, Jack Antel, and Francisco J. Quintana in PNAS. Published online February 6 2017 doi:10.1073/pnas.1615413114






